氧化和抗氧化指标在大鼠高脂饮食所致脂肪肝中的动态变化
【摘要】 目的 探讨氧应激和脂质过氧化在高脂饮食所致脂肪性肝炎形成中的作用。方法 雄性SD大鼠 30只随机分为3组,每组10只。正常组普通饲料喂养;模型Ⅰ、Ⅱ组喂高脂饲料;12周末处死正常组、模型Ⅰ组大鼠;模型Ⅱ组大鼠继续喂养至16周末处死,测定血清转氨酶(ALT、AST),全血谷胱甘肽过氧化物酶(GSH?PX),肝匀浆丙二醛(MDA)含量,超氧化物歧化酶(SOD)活性,总抗氧化能力(T?AOC),一氧化氮(NO),诱导型一氧化氮合酶(iNOS),谷胱甘肽(GSH)水平,观察肝组织学改变。结果 模型组大鼠12周出现单纯性脂肪肝,16周为脂肪性肝炎。与正常组比,模型组大鼠肝组织脂质过氧化产物MDA含量明显增多,而抗氧化物SOD,GSH,GSH?PX含量明显降低,且肝脏的脂肪变性严重程度随着高脂饮食喂养的时间延长而加剧。结论 氧应激和脂质过氧化在肝组织脂肪变性后炎症的过程中发挥重要作用。
【关键词】 氧应激 脂质过氧化 非酒精性脂肪性肝炎
Development Changes of Oxidative and Anti?oxidative Indexes in Establishment of Steatohepatitis in Rats Fed by High?fat Diets
Peng Hai?ying, Yu Hong?bo, Zuo Zhong
(Dalian Sanatorium of Shenyang Military Region, Dalian 116013, China; PLA No.210 Hospital, Dalian 116021, China)
Abstract: Objective To explore the role of oxygen stress and lipid peroxidation in the establishment of steatohepatitis in rats fed by high?fat diets. Methods Thirty male Sprague Dawley rats were assigned into three groups (n=10) at random. The rats fed by normal foods served as controls. The rats in model groups (Ⅰ, Ⅱ) were fed with high-fat diets. The animals in control group and model I group were killed at the end of the 12th week, and the ones left were killed at the end of the 16th week. Blood samples were collected for the detection of serum aspartate transaminase (AST), alanine aminotransferase (ALT) and glutathione peroxidase (GSH?PX), and liver tissues were obtained for the detection of malondialdehyde (MDA) contents, superoxide dismutase (SOD) activity, total antioxidative capacity (T?AOC), and nitric oxide (NO), inducible nitric oxide synthase (iNOS) and glutathione (GSH) levels. The histological changes were observed under light microscope. Results Pure fatty liver was formed in the model rats after in the 12th week, and fatty hepatitis was established in the 16th week. In comparison with those of normal rats, the contents of MDA were increased (P<0.01) but anti?oxide SOD, GSH, GSH?PX contents were decreased significantly (P<0.05, or P<0.01). The severity of hepatic fatty degeneration aggravated with the prolonging of the high?fat diets taking duration. Conclusion Oxidative stress and lipid peroxidation may play an important role in the formation of liver inflammation cell infiltration.
Key words: oxygen stress; lipid peroxidation; nonalcoholic steatohepatitis
研究认为氧应激和脂质过氧化在非酒精性脂肪性肝炎(nonalcoholic steatohepatitis,NASH)发病中占有重要地位[1~3]。我们通过高脂饮食建立NASH大鼠模型,动态检测氧化和抗氧化指标观察实验性NASH肝组织的氧化损伤。
1 材料和方法
1.1 材料 雄性SD大鼠 30只,体重(150±10)g,购自大连医科大学实验动物中心。胆固醇购自上海伯奥生物工程公司,猪油自备。超氧化物歧化酶(SOD)、丙二醛(MDA)、一氧化氮(NO)、诱导型一氧化氮合酶(iNOS)、总抗氧化能力(T?AOC)、谷胱甘肽过氧化物酶(GSH?PX)、还原型谷胱甘肽 (GSH)等试剂盒购自南京建成生物工程公司。
1.2 方法 大鼠普通饲料喂养1周后,随机分为3组(每组10只)。正常组普通饲料喂养;模型Ⅰ、Ⅱ组喂高脂饲料(880 g/kg普通饲料+100 g/kg 猪油+20 g/kg 胆固醇)。各组大鼠自由进食、进水,分笼(每笼5只)饲养于(20±2)℃、明暗各12 h 的动物实验室内。12周末处死正常组、模型Ⅰ组大鼠;模型Ⅱ组大鼠继续喂养至16周末处死。方法为禁食12 h,乙醚麻醉,下腔静脉采血后处死,迅速取出肝脏,按常规制备血清、肝匀浆、肝组织石蜡切片标本,肝组织于-70 ℃ 低温保存。(1)采用全自动生化分析仪测定血清ALT、AST,全血GSH?PX (DTNB直接法);(2)肝匀浆测定MDA含量(改进后的硫代巴比妥酸荧光法),SOD活性 (改良的盐酸羟胺法),T?AOC、NO、iNOS、GSH(按试剂盒说明操作);(3)肝脏病检查,光镜下评估脂肪变性程度和炎症活动度计分[4~5]。
1.3 统计学处理 计量资料以均值±标准差(±s)表示,各组间实验数据采用两样本均数的t检验;等级资料采用秩和检验。
2 结果
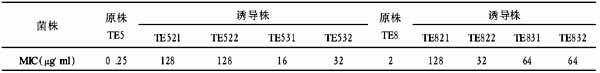
2.1 血清ALT、AST及全血GSH?PX变化 与正常组比较,模型Ⅰ,Ⅱ组ALT,AST显著增高(P<0.01),GSH?PX显著下降(P<0.01),详见表1。
表1 各组大鼠血清生化指标(略)
与正常组比较,①P<0.01
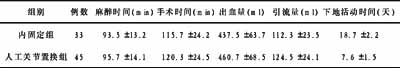
2.2 肝MDA、NO、iNOS、SOD、T?AOC及GSH变化 与正常组比较,模型Ⅰ组MDA显著增高,SOD、GSH下降明显(P<0.05);模型Ⅱ组MDA、iNOS、NO显著增高(P<0.01,P<0.05);模型Ⅱ组SOD、T?AOC、GSH增高(P<0.01),详见表2。
表2 各组大鼠肝匀浆生化指标(略)
与正常组比较,①P<0.05,②P<0.01
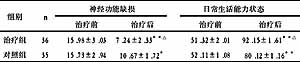
2.3 肝脏病理学变化 与正常组比,模型组大鼠肝脂肪变程度明显加重(H=11.827,P=0.003),炎症活动度计分显著增加(H=25.250,P=0.000),详见表3~4。HE染色正常组肝细胞形态正常,无脂肪变性和炎性细胞浸润;模型Ⅰ组肝组织弥漫性脂肪变性(混合型),灶状炎性细胞浸润,模型Ⅱ组见明显的桥接坏死。
表3 各组大鼠肝脂肪变性程度(略)
表4 各组炎症活动度计分比较(略)
3 讨论
越来越多的研究表明NASH与酒精性脂肪肝炎(ASH)可能存在着共同的发病机制[6]。自由基介导的肝损伤是ASH的最重要发病机制,其主要表现为氧化产物增多和(或)抗氧化作用减弱[7]。目前认为ROS大量产生引起氧应激进而导致脂质过氧化和肝脏抗氧化系统异常是NASH形成的最终共同发病机制[8~10]。来自分子氧的游离基或ROS过度产生超过肝细胞自由基清除系统对其去除能力时则产生氧应激[8,11];而因产生过量的ROS而增加的脂质过氧化是脂肪肝向NASH转化的标志[12]。本研究经过连续16周的高脂、高胆固醇饮食喂养,第12周,模型组大鼠出现明显的脂肪变性,且随着喂养时间的延长,脂肪变性的程度逐渐加重,到第16周,大鼠肝组织出现炎细胞浸润,同时转氨酶增高显著,提示病变为脂肪性肝炎阶段[13~14]。SOD是机体抗氧化损伤防御体系中的最重要的抗氧化酶;T-AOC是反映机体整体水平的抗氧化水平高低的重要指标[15];GSH是机体的另一种重要的抗氧化剂,是“抗氧化剂复合链”的主要成员之一[16];GSH-PX是机体内广泛存在的一种重要的过氧化物分解酶。我们发现模型组大鼠肝组织SOD、T?AOC、GSH下降明显,全血GSH?PX也显著降低,而脂质过氧化终产物MDA明显增高,表明NASH时产生大量的自由基和脂质过氧化物,消耗了大量的SOD、T?AOC、GSH、GSH?PX,从而使机体的抗氧化损伤的防御机制受损,不能清除过多的自由基而导致肝损伤[17]。NO在众多的氧化损伤中发挥着重要作用[18~19],而NOS是NO生成的主要限速因子。我们观察到模型组大鼠NO和iNOS含量增加,提示高脂、高胆固醇饮食可通过诱导iNOS活性,参与对肝脏的氧化损伤。综上所述,氧应激和脂质过氧化在肝组织脂肪变性后炎症的过程中发挥重要作用。因此,对NASH患者进行保肝的同时,检测脂质过氧化和抗氧化防御参数可能成为临床判定疗效和指导治疗的重要指标[20]。
【】
[ 1] Sanyal A J. AGA technical review on nonalcoholic fatty liver disease[J].Gastroenterology,2002,123:1705-1725.
[ 2] Chitturi S, Farrell G C.Etiopathogenesis of nonalcoholic steatohepatitis[J]. Semin Liver Dis,2001,21:27-41.
[ 3] Roskams T, Yang S Q, Koteish A, et al. Oxidative stress and oval cell accumulation in mice and humans with alcoholic and nonalcoholic fatty liver disease[J]. Am J Pathol,2003,163:1301-1311.
[ 4] Diel A M,Goodman Z,Ishak K G. Alcoholic liver disease in nonalcoholics. A clinical and histologic comparison with alcohol?induced liver injury[J].Gastroenterology,1998,95:1056-1062.
[ 5] 王泰龄,刘 霞,周元平,等. 慢性肝炎炎症活动度及纤维化程度计分方案[J]. 中华肝脏杂志,1998,6:195-197.
[ 6] 曾民德.脂肪肝发病机制“二次打击”假设[J].肝脏,2001,6(3):145.
[ 7] Walsh K, Alexander G.Alcoholic liver disease[J]. Postgrad Med J,2000,76:280-286.
[ 8] Angulo P. Nonalcoholic fatty liver disease[J]. N Engl J Med,2002,346:1221-1231.
[ 9] Day C P. Non?alcoholic steatohepatitis (NASH): where are we now and where are we going? [J].Gut,2002,50:585-588.
[10] Medina J, Fernandez?Salazar L I, Garcia?Buey L, et al. Approach to the pathogenesis and treatment of nonalcoholic steatohepatitis[J]. Diabetes Care,2004,27:2057-2066.
[11] Kahn B B, Flier J S. Obesity and insulin resistance[J]. J Clin Invest,2000,106(4):473-481.
[12] Younossi Z M, Diehl A M, Ong J P. Nonalcoholic fatty liver disease: an agenda for clinical research[J]. Hepatology,2002,35:746-752.
[13] Lieber C S, Leo M A, Mak K M,et al. Model of nonalcoholic steatohepatitis[J].Am J Clin Nutr,2004,79:502-509.
[14] Koteish A, Diehl A M. Animal models of steatosis[J]. Semin Liver Dis,2001,21:89-104.
[15] Salvemini D,Riley D P,Cuzzocrea S.SOD mimetics are coming of age[J].Nat Rev Drug Discov,2002,1:367-374.
[16] 海春旭. 抗氧化、抗衰老与疾病控制的研究进展[J]. 疾病控制杂志,2002,6:289-293.
[17] Koruk M, Taysi S, Savas M C,et al. Oxidative stress and enzymatic antioxidant status in patients with nonalcoholic steatohepatitis[J].Ann Clin Lab Sci,2004,34(1):57-62.
[18] Garvin J L, Ortiz P A.The role of reactive oxygen species in the regulation of tubular function[J]. Acta Physiol Scand,2003,179:225-232.
[19] Ding S P, Li J C, Jin C. A mouse model of severe acute pancreatitis induced with caerulein and lipopolysaccharide[J]. World J Gastroenterol,2003,9:584-589.
[20] Ramesh S, Sanyal A J. Evaluation and management of non?alcoholic steatohepatitis[J]. J Hepatol,2005,42(Suppl):S2-12.