IL?18基因转染对小鼠卵巢癌OVHM细胞体内成瘤的影响
作者:崔澄 郝淑维 白小嘉 李新伟 周强 程建新 单保恩
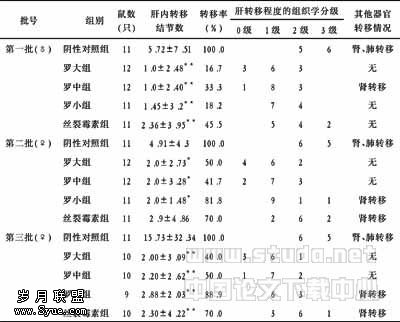
【摘要】 目的 分析转染IL?18基因后,对小鼠卵巢癌OVHM细胞体内成瘤的影响,初步探讨IL?18基因转染卵巢癌的应用价值。方法 将逆转录病毒携带的小鼠IL?18基因成功转染至OVHM(OVHM/IL?18),以空载体转染的OVHM(OVHM/LXSN)和野生型(OVHM)作为对照,于裸鼠皮下分别接种细胞,观察各组种植瘤生长情况,成瘤率;HE染色及电镜分别观察病理组织切片的形态学改变。结果 三组裸鼠的成瘤率相同,但OVHM/IL?18组成瘤时间较晚,随瘤龄增长肿瘤生长缓慢;瘤组织较小、界限清楚,血供不丰富,瘤细胞数量少、恶性程度较低,可见中性粒细胞、淋巴细胞浸润及细胞凋亡、组织坏死现象。OVHM组和OVHM/LXSN组的瘤组织较大、与周围组织界限不清,血管丰富,瘤细胞密集、恶性程度较高。结论 IL?18基因成功转染后,可能通过促进肿瘤细胞凋亡、抑制肿瘤血管形成及促进免疫浸润等机制,达到抑制肿瘤生长、降低卵巢癌恶性程度的抗瘤作用。
【关键词】 IL?18;基因转染;OVHM;成瘤;裸鼠
【Abstract】 Objective To investigate the effect of IL?18 gene transfection on tumorigenesis of mouse ovarian cancer cell line OVHM, and to discuss the preliminary value of IL?18 gene transfection in treatment of ovarian cancer. Methods OVHM was transfected with retrovirus with IL?18 gene named as OVHM/IL?18, and the wild OVHM and OVHM transfected with vector without IL?18 gene (OVHM/LXSN) were enrolled as control. The nude mice were inoculated with different cells subcutaneously, then the growth of transplanted tumor was observed, the ratios of tumorigenesis were calculated and the morphology of tumor cell in tissue was analyzed by HE staining and electron microscope. Results After inoculated respectively, the ratios of tumorigenesis were similar in three mice groups. But in OVHM/IL?18 group, the latent period of tumorigenesis was longer than that of other two groups, the slower speed along with tumor growth was observed; the tumor tissue was smaller and had a limited boundary, the number of blood vessel and tumor cells were fewer, and the malignance of tumor cells was lower;the apoptosis, coagulative necrosis and the infiltration of neutrophilic granulocytes and lymphocytes were observed. Meanwhile, the typical morphology of apoptosis was showed by electron microscope. However, the tumor tissues of OVHM and OVHM/LXSN groups were larger and had unclear boundary, the number of blood vessel and tumor cells were more, the malignance of tumor cells was higher. Conclusion Although IL?18 gene transfection successfully cannot display cytotoxicity directly in vitro, its inhibiting effects on tumorigenesis of OVHM in vivo were exerted by interdicting cell cycle and accelerating apoptosis of tumor cells, perhaps through other indirect killing pathways.
【Key words】 IL?18;Gene transfection;OVHM;Tumorigenesis; Nude mouse
白介素18(interleukin?18,IL?18)是具有抗瘤作用的重要免疫调节因子[1],随着卵巢组织从正常向良性及恶性肿瘤的转变,组织中IL?18 mRNA及蛋白表达递减直至缺如[2]。提示,若能纠正卵巢癌细胞中此因子的缺陷表达,则可有效诱导IL?18的抗瘤效应。因此,本文研究了IL?18基因成功转染至小鼠卵巢癌OVHM细胞后,对体内成瘤的影响,初步探讨使用IL?18基因对卵巢癌进行基因治疗的可行性。
1 材料与方法
1.1 细胞株、动物及主要仪器 OVHM由日本大阪大学医学院Hiromi Fujiwara博士惠赠;由逆转录病毒作为载体携带小鼠IL?18基因的PA317/IL?18、携带空载体的PA317/LXSN细胞均由日本千叶县癌症研究中心田川雅敏先生惠赠。4~6周龄BALB/c/nu雌性裸鼠(18~20)g由药品生物制品鉴定所提供(SCXK(京)2000?0010);于SPF层流室中恒温、恒湿(45%~50%)环境饲养,所用垫料、饮水、饲料等均经高压灭菌处理。G418、polybrene为美国AMRESCO公司产品;H?500型透射电镜为日本日立公司产品。
1.2 小鼠IL?18基因转染OVHM细胞 分别取达80%融合的PA317/IL?18及PA317/LXSN细胞,培养24 h后收集病毒原液上清;取对数生长期OVHM,将2×105个细胞接种于6 cm培养皿中,以终浓度400 mg/L的G418进行阳性克隆筛选,200 mg/L G418维持逐步扩大培养,20 d后分别获得转染小鼠IL?18的OVHM/IL?18和空载体转染OVHM/LXSN细胞。最后经IL?18mRNA及蛋白合成、分泌的检测,鉴定转染成功。
1.3 荷OVHM肿瘤小鼠模型的建立及成瘤观察 将15只BALB/c/nu裸鼠随机分为三组:OVHM/IL?18组,OVHM/LXSN组(空载体对照),OVHM组(野生型对照),5只/组。分别取对数生长期的细胞,于裸鼠右前肢皮下接种(2×106个/只)。每日观察小鼠的饮食、活动等一般状况及肿瘤生长情况。游标卡尺测量瘤体的长径(a)与短径(b),计算测量当日的肿瘤体积:V=a×b2/2。于接种后4周末处死,完整剥离肿瘤,称取瘤重,计算成瘤率。
1.4 荷瘤小鼠肿瘤组织的形态学观察 瘤组织经10%福尔马林固定,常规石蜡包埋切片后HE染色观察。另一部分瘤组织,经4%戊二醛?锇酸双重固定、脱水、浸透、包埋、聚合、切片、染色后,透射电镜下观察。
1.5 统计学处理 数据均以(±s)表示,采用SPSS 11.5统计软件进行方差分析。显著性检验水准α=0.05。
2 结果
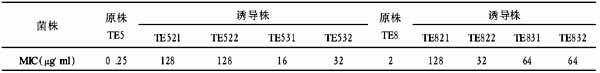
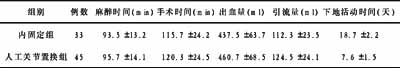
2.1 IL?18基因转染对裸鼠体内OVHM成瘤的影响 三组裸鼠的成瘤率相同,均为100%。OVHM 组及OVHM/LXSN组平均成瘤时间均为(5.5±1.2)d,随瘤龄增长肿瘤体积明显增大,裸鼠出现食欲及活动性差、倦怠等表现。OVHM /IL?18组平均成瘤时间为(10.5±1.5)d,较其他两组晚5 d左右,有显著性差异(均P<0.01);裸鼠食欲、活动情况良好;随瘤龄增长肿瘤生长缓慢,肿瘤体积和重量均较其他两组明显减小(表1、图1)。
表1 不同组别荷瘤小鼠体内肿瘤的生长(略)
分别与OVHM组及OVHM/LXSN组相比,*P<0.05;**P<0.001
图1 荷瘤4周后不同组别裸鼠体内的成瘤情况(略)
A:OVHM组 B:OVHM/LXSN组 C:OVHM/IL?18组
2.2 荷瘤小鼠肿瘤组织的形态学观察
2.2.1 大体观察 OVHM组、OVHM/LXSN组裸鼠肿瘤生长呈结节状突出于体表,瘤体较大,质脆易出血,4周后肿瘤表面相继出现破溃,浸润周围组织和皮肤,界限不清,不易分离,切面灰暗,无明显液化及坏死。OVHM/IL?18组裸鼠肿瘤组织体积较小,肿瘤表面无明显破溃,无明显周围组织浸润,易分离(见图1)。
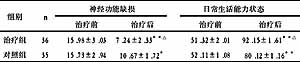
2.2.2 组织切片镜下观察 OVHM组、OVHM/LXSN组瘤组织中瘤细胞密集,胞质丰富,胞核大而深染,异型性明显,核分裂相多见;间质少,血管丰富,偶见脉管瘤栓。OVHM/IL?18组瘤细胞数目相对稀少,胞核较小,胞质少,核分裂相少见,可见散在的胞核与胞浆呈固缩坏死样改变,大片细胞坏死;间质中血管较少,可见中性粒细胞及淋巴细胞浸润(图2,见封4)。
2.2.3 电镜观察 OVHM/IL?18组裸鼠瘤细胞出现典型凋亡改变:胞核固缩,染色质边集呈新月状;胞浆浓缩并有空泡出现,可见凋亡小体;细胞器中除粗面内质网轻度扩张外,其他细胞器数量减少、体积变小;微绒毛数量减少等(图3,见封4)。其他两组瘤细胞胞质丰富,核浆比例大,可见核仁,染色质松散。
3 讨论
IL?18具有较强的抗瘤效应[3-6];卵巢癌是死亡率位居女性生殖系统肿瘤首位的妇科常见恶性肿瘤,IL?18的表达缺失在卵巢癌发生中发挥了重要作用[2]。由此推测,将IL?18基因导入卵巢癌细胞,可能对提高机体抗瘤效应有一定的应用价值。体内荷瘤结果显示,OVHM/IL?18组成瘤时间较晚,随瘤龄增长肿瘤生长缓慢,电镜观察可见典型的凋亡现象。表明,IL?18基因转染纠正卵巢癌组织的IL?18低表达状态后,可通过促进肿瘤细胞凋亡达到抑制肿瘤生长的目的。解剖及光镜观察中发现,OVHM /IL?18组瘤组织较小、界限清楚,血供不丰富,瘤细胞数量少、恶性程度较低,可见中性粒细胞、淋巴细胞浸润及细胞、组织坏死;而野生对照组和空载体组的瘤组织较大、与周围组织界限不清,血管丰富,瘤细胞密集、恶性程度较高。提示,IL?18还可能通过抑制肿瘤血管形成及促进淋巴细胞、中性粒细胞浸润,达到抑制肿瘤生长、降低卵巢癌恶性程度的抗瘤作用。而IL?18成功转染后,分别通过哪些分子机制发挥上述抗瘤作用,尚需进一步研究确定。
通过对裸鼠体内肿瘤的生长情况观察发现,OVHM/IL?18组裸鼠的肿瘤生长速度、体积及重量均明显低于对照组和空载体组,但并未表现出对肿瘤生长的完全抑制及成瘤率下降,可能是由于:①实验所用无胸腺裸鼠的T细胞免疫系统功能缺乏,而T细胞在IL?18的抗瘤活性中起重要作用[4];②肿瘤自身存在的一些免疫抑制因素可能在一定程度上抵消了IL?18的部分抗瘤作用;③是否存在荷瘤机体IL?18 表达量与其抗瘤效应之间的量效关系。因此,在后续实验中应进一步分析IL?18有效表达后,肿瘤新生血管生成、荷瘤机体免疫功能、肿瘤免疫抑制等方面的变化与肿瘤生长受抑之间的关系,以全面评价IL?18基因转染卵巢癌的可能机制途径。
【】
1 Okamura H, Tsutsui H, Komatsu T,et al.Cloning of a new cytokine that induces IFN?γ production by T cells. Nature, 1995, 378(6552):88?91.
2 Wang ZY, Gaggero A, Rubartelli A,et al.Expression of interleukin?18 in human ovarian carcinoma and normal ovarian epithelium:evidence for defective processing in tumor cells. Int J Cancer,2002,98(6):873?878.
3 Takahashi HK, Iwagaki H, Hamano R,et al.Effects of adenosine on adhesion molecule expression and cytokine production in human PBMC depend on the receptor subtype activated. Br J Pharmacol,2007,50(6):816?822.
4 Dai S, Zhou X, Wang B,et al.Enhanced induction of dendritic cell maturation and HLA?A*0201?restricted CEA?specific CD8(+) CTL response by exosomes derived from IL?18 gene?modified CEA?positive tumor cells. J Mol Med, 2006, 84(12):1067?1076.
5 Lian H, Jin N, Li X,et al.Induction of an effective anti?tumor immune response and tumor regression by combined administration of IL?18 and Apoptin. Cancer Immunol Immunother, 2007, 56(2):181?192.
6 Leng JH, Zhang LH, Yao HP,et al.Antitumor effects of interleukine?18 gene?modified hepatocyte cell line on implanted liver carcinoma. J Chin Med, 2003, 116(10): 1475?1479.