清肝活血方及其拆方对酒精性肝损伤大鼠肿瘤坏死因子α表达的影响
作者:吴涛, 柳涛, 郑培永, 邢练军, 季光
【摘要】 目的:观察清肝活血方及其拆方对酒精性肝损伤(alcoholic liver injury, ALI)大鼠肝脏肿瘤坏死因子α(tumor necrosis factor?α, TNF?α)mRNA表达和血浆TNF?α含量的影响。方法:除空白组和四氯化碳(carbon tetrachloride, CCl4)组外,80只雄性Wistar大鼠采用复合因素复制ALI模型。造模4周后将模型大鼠随机分成模型组、清肝方组、活血方组和清肝活血方组。3组予相应药物灌胃。灌胃2周后,检测血清丙氨酸氨基转移酶(alanine aminotransferase, ALT)、天冬氨酸氨基转移酶(aspartate aminotransferase, AST)活性;采用酶联免疫吸附测定法检测血浆TNF?α含量;留取肝脏标本进行苏木素?伊红染色;逆转录聚合酶链反应检测肝组织TNF?α mRNA表达。结果:清肝活血方及其拆方均可明显改善ALI大鼠肝脏脂肪变及肝脏炎症程度,清肝活血方优于清肝方。清肝活血方能显著降低模型大鼠血清ALT活性;清肝方、活血方和清肝活血方均可明显降低ALI大鼠血清AST活性,组间比较差异无统计学意义。活血方及清肝活血方能显著降低模型大鼠肝组织TNF?α mRNA表达和血浆TNF?α水平,清肝方作用不明显。 结论:清肝活血方及活血方治疗ALI的作用机制可能与减少TNF?α的产生有关。
【关键词】 清肝活血方; 清肝方; 活血方; 酒精性肝疾病; 肿瘤坏死因子α; 大鼠
Objective: To study the effects of Qinggan Huoxue Recipe (QGHXR), the compound traditional Chinese herbal medicine, and its separated recipes on the expression of tumor necrosis factor?α (TNF?α) mRNA and serum TNF?α content in rats with alcoholic liver injury (ALI).
Methods: One hundred male Wistar rats were randomly divided into normal control group (n=10), carbon tetrachloride (CCl4) group (n=10) and ALI group (n=80). Rats in the ALI group were intragastrically administered mixed liquor twice a day and intraperitoneally injected with CCl4 twice a week for 6 weeks, rats in the normal control group were intragastrically administered normal saline, and rats in the CCl4 group were intraperitoneally injected with CCl4 and olive oil twice a week continuously. Two rats in the ALI group were sacrificed for histological observation per week. After 4?week modeling, the rats in the ALI group were randomly divided into QGHXR group, Qinggan Recipe (QGR) group, Huoxue Recipe (HXR) group (15 rats in each group), and the others belonged to the untreated group. After 2?week suitable drugs treatment, the activities of serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were analyzed. Pathological changes in liver tissues were observed by HE staining. The content of plasma TNF?α was assayed by enzyme linked immunosorbent assay, and expression of TNF?α mRNA in the liver tissue was detected by reverse transcription polymerase chain reaction (RT?PCR).
Results: QGHXR and its separated recipes improved liver steatosis and inflammation, and in this regard, the QGHXR was superior to the QGR. QGHXR decreased the activity of serum ALT in rats with ALI, but QGR and HXR did not show significant effect in that. The three recipes decreased the activity of AST as compared with the untreated group, but there were no significant differences among the three treated groups. HXR and QGHXR down?regulated the expression of TNF?α mRNA in the liver tissue, but QGR did not show significant effect. HXR and QGHXR also decreased the content of plasma TNF?α, but QGR did not show significant effect in that.
Conclusion: QGHXR and HXR may provide protection against ALI in rats through decreasing the production of TNF?α.
Keywords: Qinggan Huoxue Recipe; Qinggan Recipe; Huoxue Recipe; alcoholic liver disease; tumor necrosis factor?α; rats
内毒素?库普弗细胞(Kupffer cell, KC)介导的免疫损害在酒精性肝病(alcoholic liver disease, ALD)发生中的作用日益受到重视,肿瘤坏死因子α(tumor necrosis factor?α, TNF?α)是发挥免疫损害的主要效应因子,也是重要的药物靶标。前期研究证实清肝活血方(Qinggan Huoxue Recipe, QGHXR)对ALD具有良好的治疗效果[1]。体外研究发现,清肝活血方及其拆方通过调控KC表面白细胞分化抗原14(cluster of differentiation antigen 14, CD14)和跨膜受体Toll样受体4(toll?like receptor 4, TLR4),降低TNF?α的表达,有效抑制酒精引起的肝脏损害[2]。本文进一步从体内实验证实清肝活血方及其拆方对酒精性肝损伤(alcoholic liver injury, ALI)的治疗作用及其对TNF?α表达的影响。
1 材料和方法
1.1 实验材料
1.1.1 实验动物 雄性Wistar大鼠100只,SPF级,体质量(180±10)g,购自上海斯莱克实验动物有限责任公司,许可证号为SCXK(沪)2007?0005。饲养于上海中医药大学龙华实验中心动物房。
1.1.2 药物制备 清肝活血方(柴胡9 g、黄芩9 g、丹参15 g、鳖甲9 g、葛根15 g)及其拆方清肝方(柴胡9 g、黄芩9 g)和活血方(丹参15 g、鳖甲9 g、葛根15 g),根据公式大鼠剂量=人剂量×35(人转换因子)/6(大鼠转换因子)[3],出3个方的人鼠等效剂量分别为4.75、1.5和3.25 g/kg。按传统工艺制备成水煎剂,减压浓缩至生药含量为0.475、0.15、0.325 g/ml,备用。
1.1.3 主要试剂和仪器 分析纯四氯化碳(carbon tetrachloride, CCl4)和化学纯橄榄油(国药集团化学试剂有限公司);吡唑(Fluca公司);戊巴比妥钠注射液(上海西唐生物有限公司);HE染液(上海虹桥乐翔医用试剂有限公司);TNF?α酶联免疫吸附测定(enzyme linked immunosorbent assay, ELISA)试剂盒(上海钰森生物技术有限公司);TRIzol试剂盒、逆转录聚合酶链反应(reverse transcription polymerase chain reaction, RT?PCR)试剂盒和DNA Marker(上海申能博彩生物科技有限公司);焦碳酸二乙酯(diethyl pyrocarbonate, DEPC)和琼脂糖(Sigma公司);氯仿和异丙醇(上海试剂一厂)。DY89?1型电动玻璃匀浆机,宁波新芝科器研究所产品;低温离心机,Eppendorf公司产品;iCycler PCR仪,BIO?RAD公司产品;RNA/DNA测量仪,Pharmacia公司产品;凝胶成像系统,上海四星生物技术有限公司产品;电热恒温水槽,上海精宏实验设备有限公司产品;UV?2102C型紫外可见分光光度计,UNICO公司产品;MK3型酶标仪,Thermo Labsystems公司产品。
1.2 实验方法
1.2.1 造模和给药 造模组以60度二锅头酒10 ml︰玉米油2 ml︰吡唑25 mg比例混合物灌胃,灌胃量为10 ml/(kg·d),分早、晚两次灌服。第2周开始腹腔注射CCl4和橄榄油溶液(CCl4︰橄榄油=1︰3),2次/周,每次注射0.3 ml/kg体质量,造模共6周[4]。空白组(n=10)和CCl4组(n=10)以等量生理盐水灌胃,CCl4组仅以等量CCl4橄榄油溶液腹腔注射,空白组以等量生理盐水腹腔注射。在造模的第1、2、3、4和5周各取2只模型大鼠做病理分析。造模4周后,72只模型大鼠随机分为清肝活血方组、清肝方组、活血方组各15只,余为模型组。各中药组分别予清肝活血方、清肝方、活血方灌胃,剂量为10 ml/(kg·d),共2周。模型组、空白组和CCl4组灌服等量生理盐水。
造模6周后以2%戊巴比妥钠(2 ml/kg)腹腔注射麻醉处死大鼠,腹主动脉采血,分别放于抗凝管和无抗凝剂试管中,4 ℃静置2 h,3 000 r/min 15 min,离心分离血清和血浆,-80 ℃备用。摘取肝脏称质量后,于肝右叶切取1.0 cm×1.0 cm×0.2 cm大小肝组织2块,4%中性甲醛溶液固定。剩余肝组织液氮中速冻后-80 ℃冰箱保存。
1.2.2 观察项目和方法
1.2.2.1 肝脏组织病理改变 石蜡切片,HE染色,光学显微镜下观察肝脂肪变性和炎症程度。肝细胞脂肪变性程度判断标准参照Diehl等[5]法,炎症活动度计分标准Knodell等[6]提出的慢性肝炎组织学活动指数(hepatitis histological activity index, HAI),并结合王泰龄等[7]提出的慢性肝炎炎症活动度计分方案。取两者积分总和的结果进行统计分析。
1.2.2.2 血清丙氨酸氨基转移酶和天冬氨酸氨基转移酶活性检测 血清丙氨酸氨基转移酶(alanine aminotransferase, ALT)和天冬氨酸氨基转移酶(aspartate aminotransferase, AST)活性检测均采用7170S全自动分析仪速率法进行检测。
1.2.2.3 RT?PCR法检测肝组织TNF?α mRNA表达 取肝组织100 mg按照TRIzol Reagent液说明书提取总RNA,然后用紫外分光光度计定量,检测260 nm和280 nm光密度值,确认两者比值在1.8~2.0之间,按照试剂盒说明书进行cDNA的逆转录。总RNA经RT反应后进行PCR扩增,采用AMV 20 μl体系,第一链cDNA 1 μl,10×PCR Buffer 2 μl,dNTP 1 μl,目的基因正负链各0.22 μl,β?actin正负链各0.1 μl,Taq酶0.2 μl,DEPC H2O 14.2 μl。反应条件为:95 ℃预变性5 min,95 ℃ 30 s、60 ℃ 40 s、72 ℃ 1 min,26次循环,72 ℃延伸10 min。用密度扫描仪对特异性条带进行密度扫描,测得其灰度值,其与相应的β?actin灰度值之比表示TNF?α mRNA的相对表达量。TNF?α上游序列5'?ATC GGT CCC AAC AAG GAG GAG AAG T?3',扩增片段长度166 bp;TNF?α下游序列5'?TCC TTA GGG CAA GGG CTC TTG ATG G?3',扩增片段长度545 bp。β?actin上游序列5'?TGT GAT GGT GGG TAT GGG TCA GAA G?3',扩增片段长度207 bp;β?actin下游序列5'?TCA CGG TTG GCC TTA GGG TTC AGA G?3',扩增片段长度431 bp。以上引物由上海生工生物有限公司合成。
1.2.2.4 ELISA法检测血浆TNF?α含量 按照上海钰森生物技术有限公司TNF?α ELISA检测试剂盒说明书进行。待测品孔每孔各加入待测品100 μl,充分混匀后置37 ℃ 120 min。用洗涤液将反应板充分洗涤4~6次。每孔中加入一抗50 μl。将反应板置37 ℃ 60 min,洗板。每孔加酶标抗体100 μl。将反应板置37 ℃ 60 min,洗板。每孔加入底物100 μl,置37 ℃暗处5~10 min。每孔加入50 μl终止液混匀。在492 nm处检测光密度(optical density, OD)。结果计算与判断:所有OD值都应减除空白值后再进行计算。以标准1 000、500、250、125、62.5、32、16和0 ng/L的OD值建立标准曲线。根据样品OD值在该曲线上查出相应的TNF?α含量。
1.3 统计学方法 各组计量资料以x±s表示,采用单因素方差分析进行组间比较,数据均采用SPSS 12.0软件分析,检验水准α=0.05。
2 结 果
2.1 大鼠一般状况观察 实验过程中共死亡大鼠31只,其中由于灌胃不慎致死3只,被同笼大鼠吃掉10只,酒精中毒致死18只。其中模型组死亡16只,清肝方组2只,活血方组7只,清肝活血方组6只。尸体解剖观察可见胃穿孔、胃出血、肠坏死等。空白组、CCl4组大鼠无死亡,毛发有光泽,体质量增加,体态活泼,食量及二便正常,无嗜睡和精神萎靡现象。模型组大鼠每天灌酒后出现暂时性兴奋,很快出现醉酒状态并开始酣睡,皮毛疏松无光泽,精神不振,而且饮食逐渐减少,体质量增长缓慢,大便溏泻,小便黄。各中药组大鼠醉酒状和精神不振状态有所减轻,食量增加,体质量增长明显,大便溏泻和小便黄的情况明显改善。
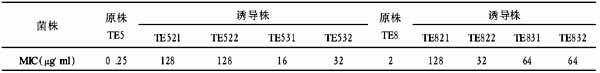
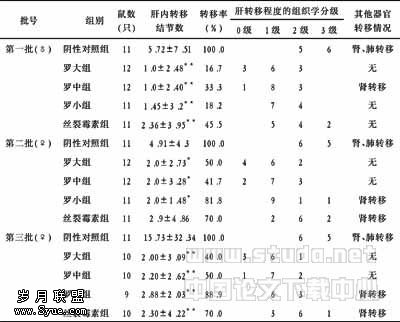
2.2 大鼠肝脏病理变化 空白组大鼠肝小叶结构清晰,肝细胞索排列整齐,呈放射状,肝窦正常,胞核结构清晰。模型组大鼠造模第6周后肝细胞脂变更加明显,肝细胞肿大,胞浆疏松化,肝细胞内出现大量小脂滴空泡,核被挤向边缘,同时伴有炎性细胞浸润,肝脏脂肪变等;肝脏炎症积分与空白组比较,差异有统计学意义(P<0.01)。CCl4组大鼠表现与空白组基本相同。清肝活血方及其拆方均可明显改善ALI大鼠肝脏脂肪变及肝脏炎症程度,与模型组比较,其积分差异有统计学意义(P<0.01),且清肝活血方优于清肝方(P<0.05)。见表1和图1。
2.3 大鼠血清ALT和AST活性的变化 模型组大鼠血清ALT、AST活性较空白组升高(P<0.01,P<0.05);CCl4组ALT活性与空白组比较无明显改变,AST活性明显升高(P<0.05);清肝活血方能显著降低模型大鼠血清ALT活性(P<0.01),清肝方和活血方无明显作用;清肝方、活血方和清肝活血方均可明显降低ALI大鼠血清AST活性(P<0.05,P<0.01),3治疗组组间比较差异无统计学意义。见表2。表1 清肝活血方及其拆方对ALI大鼠肝脏脂肪变性及肝脏炎症程度的影响表2 清肝活血方及其拆方对ALI大鼠血清ALT和AST活性的影响
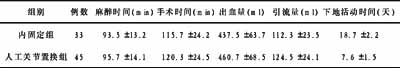
2.4 大鼠肝组织TNF?α mRNA表达的变化 空白组肝脏组织TNF?α mRNA表达较低;模型组大鼠肝脏组织TNF?α mRNA表达较空白组显著增强(P<0.01);CCl4组与空白组比较无明显改变;活血方及清肝活血方能显著降低模型大鼠TNF?α mRNA表达(P<0.01,P<0.05),清肝方作用不明显。见图2。
2.5 大鼠血浆TNF?α含量的变化 与空白组比较,模型组大鼠血浆TNF?α水平明显升高(P<0.01);CCl4组无明显改变;活血方和清肝活血方可明显降低模型大鼠血浆TNF?α水平(P<0.01),清肝方作用不明显。见表3。表3 清肝活血方及其拆方对ALI大鼠血浆TNF?α含量的影响
3 讨 论
TNF?α主要由单核巨噬细胞、肝星状细胞(hepatic stellate cells,HSC)和KC等产生,具有促炎症活动及细胞毒性作用。TNF?α是一个重要的细胞因子,在各种原因引起的肝脏损伤、HSC活化以及肝细胞再生过程中均发挥重要作用[8, 9]。Thurman[10]对ALD研究显示,长期肠内乙醇刺激使KC对脂多糖(lipopolysaccharide, LPS)刺激敏感性增加,产生的炎症介质尤其是TNF?α增加,导致进一步的肝脂肪变、炎症及肝纤维化,严重地损伤肝脏功能。Su等[11]提出,在ALD形成过程中关键的中介者可能是早期由肝脏中的KC所产生的细胞因子TNF?α、脂多糖结合蛋白(lipopolysaccharide binding protein, LBP)和CD14等。TNF?α是一种有免疫活性的细胞因子,它不仅与IL?6、IL?1形成重要的炎症介质,而且还能刺激HSC的增殖,促使HSC产生细胞外基质(extracellular matrix, ECM)[12, 13]。研究显示,TNF?α能促使活化的HSC自分泌多种细胞因子,如IL?6、IL?1、表皮生长因子(epidermal growth factor, EGF)、内皮素?1(endothlin?1, ET?1)和转化生长因子(transforming growth factor, TGF)等,后者再次激活HSC,使其产生大量的ECM,加重肝纤维化的进展[14]。因此减少TNF?α的合成或拮抗其作用可以显著降低各种原因所致的肝脏损伤程度[15, 16]。
本研究基于前期良好的临床及药效学研究基础,从细胞因子的角度探讨清肝活血方及其拆方ALI的作用机制。结果显示,模型组大鼠TNF?α mRNA表达量明显高于正常组;清肝活血方和活血方明显减少模型大鼠TNF?α mRNA表达量,清肝方效果不明显。TNF?α蛋白分泌与TNF?α mRNA表达趋势类似。提示清肝活血方、活血方可有效抑制TNF?α的产生,而清肝方对TNF?α基因和蛋白的调控不明显。
研究发现,凡是能够中和TNF?α作用和影响TNF?α产生或功能的方法都会在一定程度上保护肝脏,降低死亡率[17]。有研究证实,在多种急慢性实验性肝损伤时,TNF?α表达和血清水平显著增加,给动物注入TNF?α可产生与LPS相同的肝损害,加入TNF?α单克隆或多克隆抗体可使肝损伤显著减轻,给受到肝毒性损害的动物注射可溶性TNF?α受体,可显著降低转氨酶,减轻肝组织损伤,降低死亡率[18]。郑晓宾等[19]研究认为,丹参可以增强KC吞噬能力,有效清除自由基,抑制KC发生“呼吸爆发”从而减少细胞因子的释放;许锋等[20]研究表明丹参和丹参素对LPS刺激下KC分泌的多种细胞因子IL?1、IL?6和TNF?α有明显的抑制作用。清肝活血方及活血方发挥对ALI的防治作用,其作用机制可能与减少TNF?α的产生有关。
活血方主要由丹参、葛根和鳖甲组成。实验结果显示,活血方可以抑制效应产物TNF?α的产生。内毒素血症时,内毒素激活KC,使其释放TNF?α和干扰素等,这些细胞因子也能引起ET?1的合成和释放增加[21],提示TNF?α间接参与血瘀形成。也有研究认为TNF?α能直接抑制纤溶系统以促进血凝,还能引起微血管舒缩异常和微血栓形成,实验模型中动物的血瘀征象可能和TNF?α有密切关系[22]。实验研究显示,注入LPS 12 h后,TNF?α明显增加,而经地塞米松和活血化瘀药治疗后,TNF?α有所减少,以活血化瘀药效果显著[23, 24]。刘庆生等[25]研究发现活血药物三七能显著降低ALI大鼠血清TNF?α水平,这可能是其有效防治ALI的发生的重要机制之一。活血化瘀药物有下调促炎症细胞因子IL?6、TNF?α产生,对血小板及毛细血管内皮细胞的毒性损害具有明显的治疗和保护效应[26, 27]。这些研究同本研究结果相似,用此推测活血方有可能是通过抑制TNF?α的产生来发挥活血化瘀作用。
【】
1 Ji G. Clinical study on treatment of alcoholic liver disease by Qinggan Huoxue Recipe. Zhong Xi Yi Jie He Xue Bao. 2003; 1(2): 103?107, 124. Chinese with abstract in English.
季光. 清肝活血方治疗酒精性肝病的临床研究. 中西医结合学报. 2003; 1(2): 103?107, 124.
2 Ji G, Wang M, Zheng PY, et al. Effects of Qinggan Huoxue Recipe and its decomposed formulas on CD14, Toll like receptor 4 and nuclear factor?κB expressed by Kupffer cells. Zhong Xi Yi Jie He Xue Bao. 2006; 4(5): 509?513. Chinese with abstract in English.
季光, 王淼, 郑培永, 等. 清肝活血方及其拆方对库普弗细胞表达CD14、Toll样受体4和核因子κB的影响. 中西医结合学报. 2006; 4(5): 509?513.
3 Wang L, Ji G, Zheng PY, et al. Establishment of a rat model of alcoholic liver fibrosis induced by complex factors. Zhong Xi Yi Jie He Xue Bao. 2006; 4(3): 281?284. Chinese with abstract in English.
王磊, 季光, 郑培永, 等. 大鼠酒精性肝纤维化复合模型的建立. 中西医结合学报. 2006; 4(3): 281?284.
4 Zhang DF. Experiments of pharmacology and traditional Chinese medicine pharmacology. Shanghai: Shanghai Scientific and Technical Publishers. 2002: 8?10. Chinese.
张大方. 药理与中药药理实验. 上海: 上海技术出版社. 2002: 8?10.
5 Diehl AM, Goodman Z, Ishak KG. Alcohollike liver disease in nonalcoholics. A clinical and histologic comparison with alcohol?induced liver injury. Gastroenterology. 1988; 95(4): 1056?1062.
6 Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981; 1(5): 431?435.
7 Wang TL, Liu X, Zhou YP, et al. A semiquantitative scoring system for assessment of hepatic inflammation and fibrosis in chronic viral hepatitis. Zhonghua Gan Zang Bing Za Zhi. 1998; 66(4): 195?197. Chinese with abstract in English.
王泰龄, 刘霞, 周元平, 等. 慢性肝炎炎症活动度及纤维化程度计分方案. 中华肝脏病杂志. 1998; 66(4): 195?197.
8 Marra F. Chemokines in liver inflammation and fibrosis. Front Biosci. 2002; 7: d1899?d1914.
9 Diehl AM. Liver regeneration. Front Biosci. 2002; 7: e301?e314.
10 Thurman RG. Mechanisms of hepatic toxicity Ⅱ. Alcoholic liver injury involves activation of Kupffer cells by endotoxin. Am J Physio1. 1998; 275(4 Pt 1): G605?G611.
11 Su GL, Rahemtulla A, Thomas P, et al. CD14 and lipopolysaccharide binding protein expression in a rat model of alcoholic liver disease. Am J Pathol. 1998; 152(3): 841?849.
12 Andus T, Geiger T, Hirano T, et al. Action of recombinant human interleukin 6, interleukin 1 beta and tumor necrosis factor alpha on the mRNA induction of acute?phase proteins. Eur J Immunol. 1988; 18(5): 739?746.
13 Faouzi S, Lepreux S, Bedin C, et al. Activation of cultured rat hepatic stellate cells by tumoral hepatocytes. Lab Invest. 1999; 79(4): 485?493.
14 Maher JJ, Lozier JS, Scott MK. Rat hepatic stellate cells produce cytokine?induced neutrophil chemoattra?ctant in culture and in vivo. Am J Physiol. 1998; 275(4 Pt 1): G847?G853.
15 Reeves HL, Friedman SL. Activation of hepatic stellate cells??a key issue in liver fibrosis. Front Biosci. 2002; 7: d808?d826.
16 Diehl AM. Tumor necrosis factor and its potential role in insulin resistance and nonalcoholic fatty liver disease. Clin Liver Dis. 2004; 8(3): 619?638.
17 Bruck R, Shirin H, Hershkoviz R. Analysis of Arg?Gly?Asp mimetics and soluble receptor of tumour necrosis factor as therapeutic modalities for concanavalin A induced hepatitis in mice. Gut. 1997; 40(1): 133.
18 Czaja MJ, Xu J, Alt E. Prevention of carbon tetrachloride?induced rat liver injury by soluble tumor necrosis factor receptor. Gastroenterology. 1995; 108(6): 1849?1854.
19 Zheng XB, Han DW, Xu RL, et al. Radix salviae miltiorrhizae protects experimental acute hepatic injury by inhibiting tumor necrosis factor?α production. Zhongguo Mian Yi Xue Za Zhi. 1997; 13(3): 157?158. Chinese with abstract in English.
郑晓宾, 韩德五, 许瑞龄, 等. 丹参防治实验性急性肝损伤机制的研究. 免疫学杂志. 1997; 13(3): 157?158.
20 Xu F, Lu BG, Yao Z, et al. Effects of red sage root and danshensu on the kinetics of cytokines secreted by hepatic macrophages and the possible mechanism. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 1996; 8(5): 262?265, 318. Chinese with abstract in English.
许锋, 陆伯刚, 姚智, 等. 丹参及丹参素对内毒素刺激下肝巨噬细胞分泌细胞因子影响的动态观察. 中国危重病急救医学. 1996; 8(5): 262?265, 318.
21 Xu YS, Li YY, Wang DH, et al. Clinical and experimental study about the Jiedu Huayu Recipe in treating endotoxemia of seasonal febrile disease. Zhongguo Yi Yao Xue Bao. 1990; 5(3): 15?19. Chinese.
徐应抒, 李跃英, 王德华, 等. 解毒化瘀汤治疗温病内毒素血症的临床与实验研究. 中国医药学报. 1990; 5(3): 15?19.
22 Cheng ZQ, Du J. Experimental research on the relations between acute heat stasis syndrome in seasonal febrile disease and TNF?α, ET?1. Zhongguo Zhong Yi Ji Chu Yi Xue Za Zhi. 2001; 7(11): 25?28. Chinese with abstract in English.
程志强, 杜健. 温病急性热瘀证与TNF?α、ET?1的相关性实验研究. 中国中医基础医学杂志. 2001; 7(11): 25?28.
23 He SL, Yang XP, Peng ZP, et al. Experimental study of complex Salvia miltiorrhiza injection in treating endotoxin shock. Zhong Yi Za Zhi. 1983; 24(8): 75. Chinese.
贺石林, 杨锡平, 彭芝配, 等. 复方丹参液抗内毒素休克的实验研究. 中医杂志. 1983; 24(8): 75.
24 Xu F, Chen BG, Yao Z, et al. Dynamic observation of the effect of Rhubarb and emodin on the cytokines secreted by Kupffer cells under the endotoxin excitation in rats. Zhongguo Shi Yan Lin Chuang Mian Yi Xue Za Zhi. 1996; 8(5): 41?43. Chinese.
许锋, 陈伯刚, 姚智, 等. 大黄、大黄素对内毒素刺激下大鼠肝巨噬细胞分泌细胞因子影响的动态观察. 中国实验临床免疫学杂志. 1996; 8(5): 41?43.
25 Liu QS, Wang XQ, Lai LQ, et al. Effects of Sanchi on hepatic expression of TNF?α in alcoholic hepatopathy rats. Zhonghua Zhong Yi Yao Xue Kan. 2008; 26(2): 317?320. Chinese with abstract in English.
刘庆生, 王小奇, 来立群, 等. 三七对酒精性肝病大鼠肝组织学和TNF?α影响. 中华中医药学刊. 2008; 26(2): 317?320.
26 Cao SH, Gao HM, Wang YQ, et al. Effect of Shennong 33 on the cytokine of rats with multiple organ dysfunction syndrome. Zhonghua Ji Zhen Yi Xue Za Zhi. 2003; 12(2): 94?96. Chinese with abstract in English.
曹书华, 高红梅, 王永强, 等. "神农33号"对多器官功能障碍综合征大鼠细胞因子的影响. 中华急诊医学杂志. 2003; 12(2): 94?96.
27 Yang HX, Bai JW, Zhang H, et al. Effect of activating microcirculation and removing blood stasis medicinal herbs on the releasing of cytokines in endotoxin shock in rat. Zhongguo Zhong Xi Yi Jie He Ji Jiu Za Zhi. 2001; 1(8): 6?8. Chinese with abstract in English.
杨海贤, 白景文, 张宏, 等. 活血化瘀药对内毒素休克大鼠细胞因子释放的影响. 中国中西医结合急救杂志. 2001; 1(8): 6?8.