盆腔脂肪增多症1例报告及文献复习
作者:赵振蒙,李 凌,马鸿钧,冯 波,董泽泉,申吉泓
【摘要】 目的 提高盆腔脂肪增多症的认识。方法 盆腔脂肪增多症1例,男,32岁。影像学检查:B超及IVU示双肾中度积水,双侧输尿管全程扩张。后尿道延长,膀胱呈“竖直灯泡”状改变。结肠气钡双重造影:乙状结肠及直肠上段向后受压变细。CT示:盆腔内均匀低密度脂肪堆积。双肾盂、肾盏及输尿管扩张明显,前列腺位置抬高。尿动力学检查:最大尿流率25.3ml/s,排尿量114ml,残余尿300ml。膀胱测压;膀胱顺应性正常,非抑制性收缩波较多,逼尿肌功能正常。尿道压正常。采用硬膜外麻醉下剔除膀胱及输尿管周围脂肪组织,松解输尿管下段及双侧输尿管置管方法。结合复习讨论盆腔脂肪增多症的特点。结果 硬膜外麻醉下先拟行双侧输尿管置管,进镜后见精阜与膀胱颈间距>10cm,内有多个息肉样物,未找到输尿管开口。退镜后改平卧位,探查见盆腔内膀胱及乙状结肠周围充满大量脂肪组织,与影像学表现一致。剔除膀胱及输尿管周围多余脂肪组织。同时行双侧输尿管松解。打开膀胱,找到双侧输尿管开口,分别插入8F单“J”管。输尿管管口周围有多个息肉,约1cm×1cm大小,分别电灼之。术后病理报告:盆腔增生纤维,脂肪组织中原壁血管增生。术后1周下床活动,4周拔除双侧单“J”管。分别于术后一周和3个月复查B超和IVU,双肾盂积水和双侧输尿管扩张逐渐减轻。结论 B超、X线、CT为本病的主要诊断依据。开放手术剔除膀胱及输尿管周围脂肪,同时行双侧输尿管松解及置管术是治疗本病的有效方法。
【关键词】 盆腔脂肪增多症;手术
【Abstract】 Objective To improve the awareness of pelvic lipomatosis in clinical practice. Methods A 32-year-old male patient with pelvic lipomatosis was admitted. Imaging studies: There were mid-degree of hydronephrosis both side on B ultrasonography and IVU, and a typical“vertical bulb”shape of bladder and extended posterior were also seen on IVU. The sigmoid colon and upper rectum were pressed backward and narrowed on colic photography. CT scan showed that low density lipid piled in the pelvic cavity. The bilateral renal pelvix and ureter were markedly dilated, the prostate gland was lifted up. Urodynamic examination: The max flow rate 25.3ml/s, urine volume 114ml, residual urine 300ml.The bladder was with increased non-inhibited contract wave, normal resilience and dribbling muscle. The urethral pressure was normal. The lesions in the pelvic cavity and around the ureters were removed and the lower segments of the ureters were loosened under extradural-anesthesia, after which double J tube were placed into the ureters. The clinical characteristics of lipomatosis were reviewed by combination with the literature. Results Under extradural-anesthesia, the cystoscope was placed into the bladder, the seminal colliculus and bladder neck were seen with their distance larger than 10 cm. There were multiple polypoid tissue in the bladder. The bilateral catheterization of ureters can not be carried out because of no finding of the ureter orifice. After taking out of the cystoscope, the patient was taken to decubitus position. Intraoperatively, apparently increased lipid tissue was found in the pelvic cavity and there was large amount of lipid tissue filling the space around bladder, rectum and sigmoid colon, which was consistent with the imaging study findings. Superfluous lipid tissue around the bladder and ureter was removed, synchronously the lower ureters were loosened. Single J tubes (8F) were placed into bilateral ureters. The polyp around the ureter orifice which were about 1cm×1 cm were electronically cauterized. Pathologic study: hyperplastic fibrous tissue in pelvic cavity, Hyperplastic capillary vessel in lipid tissue. The patient was discharged 1 week after surgery, and the single J tubes were pulled out after 3 more weeks. Hydronephrosis and dilation of ureters were gradually relieved according to B ultrasonography and IVU done after 1 week and 3 months. Conclusion B ultrasonography, X-ray and CT scan are the most valuable examination in diagnosis of lipomatosis. Removing the lipid in the pelvis and around the bladder and loosening the ureters, then ureters catheterization by opening operation are effective treatment of pelvic lipomatosis.
【Key words】 pelvic lipomatosis; surgery
盆腔脂肪增多症为一种病因未明的良性罕见病。1959年Engels首次描述此病,Fogg和Smyth于1968年正式命名此症,定义为直肠与膀胱周围盆腔空间内正常脂肪组织的过度增生[1]。2004年8月我们收治1例,采用盆腔及输尿管周围脂肪剔除及双侧输尿管置管术,疗效满意。结合文献复习讨论。现报告如下。
1 临床资料
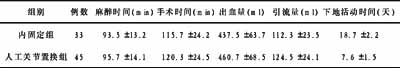
1.1 病例资料 患者,男,32岁。因“反复腰背痛伴尿频,尿急5年,大便变细2年”于2004年8月18日入院。2年前因“肾结石”服中药后排出0.5cm结石一枚。查体:血压120/80mmHg,身高175cm,体重75kg。下腹饱满,腹软,未触及包块。(直肠指诊:前列腺位置抬高,只触及前列腺尖部。)生化检查肾功能正常。影像学检查:B超可见双肾中度积水,双侧输尿管全程扩张,最大直径1.1cm。KUB加IVU:双肾中度积水,双输尿管全程扩张。CT:盆腔内均匀低密度脂肪堆积。双肾盂、肾盏及输尿管扩张明显,前列腺位置抬高。膀胱镜不能置入膀胱。膀胱尿道造影:尿道注入造影剂,见后尿道延长。膀胱显影,呈“竖直灯泡”状改变,密度均匀,边缘光滑,未见充盈缺损。排尿观察:膀胱收缩良好,膀胱颈部呈梭形改变,上抬受压。结肠气钡双重造影:乙状结肠及直肠上段向后受压变细,管壁光滑,黏膜连续,未见破坏,中断。 尿动力学检查:最大尿流率25.3ml/s,排尿量114ml,残余尿300ml。膀胱测压;膀胱顺应性正常,非抑制性收缩波较多,逼尿肌功能正常。尿道压正常。
1.2 治疗方法及结果 硬膜外麻醉下先拟行双侧输尿管置管,进镜后见精阜与膀胱颈间距大于10cm,内有多个息肉样物,膀胱黏膜光滑,未找到输尿管开口。退镜后改平卧位,下腹正中切口,探查见膀胱明显抬高,膀胱周围脂肪较多,切除膀胱前及双侧后壁脂肪,于右侧找到扩张的右输尿管,向下分离并剔除输尿管周围多余的脂肪直至近膀胱入口处。同法剔除左侧输尿管及周围的多余脂肪。剔除过程中见脂肪组织较硬,血运丰富,纤维较多,粘连。打开膀胱,未见双侧输尿管开口,但见尿液经膀胱颈口内流出,切开颈口找到双侧输尿管开口,分别插入8F单“J”管。管口周围有多个息肉,均1cm大小,分别电灼之。术后病理报告:盆腔增生纤维,脂肪组织中原壁血管增生。(术后1周下床活动,4周拔除双侧单“J”管。分别于术后1周和3个月复查B超和IVU,双肾盂积水和双侧输尿管扩张逐渐减轻。)患者无不适症状,目前仍在随访中。
2 讨论
盆腔脂肪增多症是一种大量脂肪组织增生堆积于盆腔,挤压、包绕压迫及牵引局部脏器,使器官变形狭窄或移位,从而产生以泌尿系及下消化道症状为主的良性病变。
2.1 流行病学及病因 本病临床罕见,发病年龄多数在20~60岁之间[2]。病因不明,有学者认为与慢性泌尿系统感染所致的盆腔炎症、激素代谢紊乱、先天性静脉血管异常有关[2]。有学者认为本病是肥胖的局部表现[3]。一组51例患者资料显示65%的患者有不同程度的肥胖,29%根本没有肥胖,6%为瘦弱[2]。也有学者认为本病与肥胖无关[2]。Battista[4]等动物实验证明带有截短的HMGI-C(high mobility group)基因的转基因大鼠表现为一种以腹部或盆腔脂肪增多症占优势的巨大表型,认为可能与HMGI-C基因有关;在人类包括脂肪瘤的各种良性间质肿瘤发现了12号染色体上的HMGI-C基因发生易位[4,5]。Tong等[6]报道越南籍兄弟2人均患有盆腔脂肪增多症。国内报道1例合并先天性隐睾、多发性肠源囊肿[3]。Kume等[7]报道软骨发育不全并发盆腔脂肪增多症,而软骨发育不全属先天性遗传性疾病。因此,推测盆腔脂肪增多症可能与先天或遗传因素有关。
2.2 病理 盆腔脂肪增多症是一种少见的原因不明的良性瘤样病变,病理特征为盆腔脂肪组织大量堆积,特点是膀胱、前列腺及直肠周围脂肪组织不正常增生,无境界及包膜,罕见情况下可伴腹腔内及腹膜后脂肪增多。镜下可见为成熟的脂肪组织,有时在增生的脂肪组织中,可见纤维结缔组织增生及炎性细胞浸润[8]。
2.3 临床表现及诊断 本病患者多因并发症而就诊,约有50%的患者主诉有泌尿系症状,22%有胃肠症状。泌尿系症状出现频率最高为尿频、排尿困难和夜尿增多
2.4 鉴别诊断 盆腔脂肪增多症应与盆腔畸胎瘤、脂肪瘤、腹膜后纤维化、脂肪肉瘤鉴别,前两者症状较局限,虽可见脂肪征象团块,但有完整包膜、边界清,且无膀胱形态改变;畸胎瘤密度欠均,常伴有钙化;巨大脂肪瘤可呈分叶状;腹膜后纤维化为腹膜后广泛病变,病变组织无脂肪特征。故主要应与脂肪肉瘤鉴别,脂肪肉瘤病情进展快,呈恶病质,早期血行转移,症状出现早,CT见病变范围广,其内常有软组织密度灶,而没有脂肪密度,有直接侵犯周围脏器征象,而非单纯压迫[14]。CT、MRI较易对上述疾病鉴别,可作为首选。
2.5 由于本病的病因及病程不明,治疗存在争议,目前尚无公认的有效治疗措施。本病为良性疾病,多数进展缓慢,但也可在短期内因肾积水、肾功能不全终需行尿流改道术。综合当前治疗主要分为保守治疗与手术治疗。
2.5.1 保守治疗 国内外虽有各种保守治疗方法获一定疗效的报道,包括长期口服抗生素、饮食控制等[2],但都为个案报道且随访时间短,疗效甚微且不确切。激素治疗和外放射治疗国外有学者报道,效果不佳[9]。
2.5.2 手术治疗 外科手术主要针对其尿路梗阻造成严重积水或严重的乙状结肠梗阻,理想的方法为手术剔除多余脂肪组织,松解下段狭窄输尿管,但由于本症增多的脂肪组织血运较丰富,富含纤维且与盆腔脏器粘连,术中难以找到剥离平面,手术易造成盆腔脏器损伤。多数学者主张尿流改道、经尿道切除前列腺或膀胱颈口等手术。Klein等[9]主张将患者分为年轻组和老年组,前者多较健壮,有膀胱形态改变及膀胱刺激症状,病情发展较快,较早出现尿路梗阻或尿毒症,应较早外科干预。后者病情发展较缓慢,可10年或更长无病情变化,应定期随访,半年1次肾功能检查,每两年1次造影检查,及定期膀胱镜检,必要时手术。国内外有零星报道开放性盆腔脂肪切除术治疗后随访无复发,程继义等[15]报道4例其中1例行开放手术剔除膀胱周围过多的脂肪组织,松解两侧盆部输尿管至入膀胱处,随访8个月疗效较好。李锋等[16]亦报道1例术后血压恢复正常。Halachmi等[17]报道1例开放手术松解切断输尿管于膀胱顶吻合,并采用整形外科的超声油脂仪抽吸脂肪组织,也获得了较好的效果。
本病手术治疗的关键为保护输尿管血运,以免输尿管血供不足造成尿瘘或损伤输尿管,术后留置盆腔引流管充分引流,同时选用有效抗生素防感染。本例除手术剔除膀胱周围过多的脂肪组织,松解两侧输尿管至膀胱入口处,亦打开膀胱,行膀胱颈内切开,双侧输尿管置管,术后恢复顺利,无并发症,近期疗效满意。但患者以后能否不再复发及进展,有待长期随访观察。
【文献】
1 周良平,蒋学祥,王霄英,等. 盆腔脂肪增多症的MRI诊断. 医学影像技术,2003,19:450-453.
2 Heyns CF. Pelvic lipomatosis: a review of its diagnosis and management. J Urol, 1991, 146: 267-273.
3 李庆生,曹结水,汪秀爱,等. 盆腔脂肪增多症的CT、MRI诊断. 安徽医科大学学报,1998,33:316-317.
4 Battista S, Fidanza V, Fedel M, et al. The expression of a truncated HMGI-C gene induces gigantism associated with lipomatosis. Cancer Res, 1999, 59: 4793-4797.
5 Hess JL. Chromosomal translocations in benign tumours: the HMGI proteins. Am J Clin Pathol, 1998, 109: 251-261.
6 Tong RB, Larner T, Finlay M, et al. Pelvic lipomatosis associated with proliferative cystitis occurring in the brothers. Urology, 2002, 59: 602vxii-xx.
7 Kume H, Kume Y, Takamoto K. Achondroplasia associated with pelvic lipomatosis. Lancet, 1999, 353: 1017-1019.
8 同济医科大学病教研室、中山医科大学病理学教研室.外科病理学,第2版. 武汉:湖北技术出版社,1999,318-322.
9 Klein FA, Smith MJ, Kasenetz J. Pelvic lipomatosis: 35-years experiences. J Urol, 1988, 139: 998-1001.
10 Moss AA, Clark RE, Goldberg HE, et al. Pelvic lipomatosis: a roentgen graphic diagnosis. AJR, 1972, 115: 441-445.
11 Gerson ES, Gerzof SG, Robbins AH. CT confirmation of pelvic lipomatosis: two cases. AJR, 1977, 129: 338-340.
12 李善军,毕东滨,王法成,等. 盆腔脂肪增多症的影像学诊断. 医学影像学杂志,2003,13:494-496.
13 Yalla SV, Ivker M, Burros HM, et al. Cystitis glandularis with perivesical lipomatosis: frequent association of two unusual proliferative congitions. Urology, 1975, 5: 383-386.
14 Andac N, Baltacioglu F, Cimsit NC, et al. Fat necrosis mimicking liposarcoma in a patient with pelvic lipomatosis, CT findings. Clin Imaging, 2003, 27: 109-111.
15 程继义,王法成,尉立京,等. 盆腔脂肪增多症四例报告. 中华泌尿外科杂志,1997,18:301-303.
16 李锋,刘铭,苏旭,等. 盆腔脂肪增多症2例. 临床泌尿外科杂志,2000,15:215-217.
17 Halachmi S, Moskovitz B, Calderon N, et al. The use of an ultrasonic assisted lipectomy device for the treatment of obstructive pelvic lipomatosis. Urology, 1996, 48: 128-130.