286例非酒精性脂肪肝患者血液生化指标和肝纤维化指标的分析
作者:肖桂初,黄维加,刘键,李振华,肖晓友,莫凡
【关键词】 非酒性脂肪肝;血液生化指标;肝纤维化指标
[摘要] 目的:探讨血液生化和肝纤维化指标在非酒精性脂肪肝患者临床诊断中的意义。方法:对符合B超诊断的286例非酒精性脂肪肝患者进行血液生化指标(TG、TC、HDLc、LDLc、ALT、AST、GGT、ALP)和肝纤维化指标(PCⅢ、HA、CⅣ、LN)检测,并以体检健康者作为对照。结果:非酒精性脂肪肝患者TG和TC水平均高于对照组(P<0.01),HDLc和LDLc与对照组相比分别呈下降和升高的趋势;重度非酒精性脂肪肝组ALT、AST和GGT明显升高(P<0.01),ALP升高不显著(P>0.05);非酒精性脂肪肝患者PCⅢ、HA、CⅣ和LN均高于健康组(P<0.05),重度组与轻、中度组之间PCⅢ、HA、CⅣ和LN差异均有显著性(P<0.01),中度脂肪肝与轻度脂肪肝之间PCⅢ、HA、CⅣ和LN差异无显著性(P>0.05)。结论:非酒性脂肪肝患者多项血液生化指标异常,重度非酒性脂肪肝患者尚存在不同程度的肝纤维化趋向。多项血液生化指标的检测可作为非酒精性脂肪肝筛查的重要依据,而肝纤维化指标的检测可进一步作为非酒精性脂肪肝病情监控和疗效评估的重要依据。
[关键词] 非酒性脂肪肝;血液生化指标;肝纤维化指标
Assessment of the Clinical Significance of Serum Biochemistry and Liver Fibrosis
Indexes in 286 Patients with Nonalcoholic Fatty Liver Disease
Abstract:Objective To assess the clinical significance of serum biochemistry and liver fibrosis indexes in the patients with nonalcoholic fatty liver disease.Methods Biochemistry indexes,TG,TC,HDLc,LDLc,ALT,AST,GGT and ALP,and liver fibrosis indexes,PCⅢ,HA,CⅣ and LN,were determined in 286 patientes with nonalcoholic fatty liver disease diagnosed with B ultrasonic echography,and take 100 normal volunteer as control.Results Serum TG and TC levels in the patients with nonalcoholic fatty liver disease were much higher than those in the control.Serum HDLc level was increased,but LDLc level was decreased in the patients with nonalcoholic fatty liver disease.Serum ALT,AST and GGT levels in severe fatty liver cases were significantly raised and the serum ALP levels were not raised.Serum level of PCⅢ,HA,CⅣ and LN in the patients with nonalcoholic fatty liver disease were significantly higher than those of heathy subjects.the differences of PCⅢ,HA,CⅣ and LN between the patients with severe and moderate or mild fatty liver disease were significant.But the difference of PCⅢ,HA,CⅣ and LN between the patients with mild and moderate fatty liver disease was not significant.Conclusion Multiple biochemical indexes were abnormal in the patients with nonalcoholic fatty liver disease,and the patients with severe nonalcoholic fatty liver disease has a trend of liver fibrosis.Determination of multiple biochemical indexes could provide a useful tool for Screening nonalcoholic fatty liver disease.Moreover,the detection of Liver fibrosis indexes may be helpful in the monitoring and assessing curative effect of this disease.
Key words:Nonalcoholic fatty liver disease;Biochemical indexes;Liver fibrosis indexes
非酒精性脂肪肝(nonalcoholic fatty liver disease,NAFLD)是一类肝组织学改变与酒精性肝病相类似,但无过量饮酒史的临床病理综合征,包括单纯肝细胞脂肪变性和脂肪性肝炎。以往认为它是一种良性疾病,但是在部分患者中非酒精性脂肪性肝炎(nonalcoholic steatohepatitis,NASH)可进展为肝纤维化、肝硬化和终末期肝病[1]。近年来随着肥胖、糖尿病及高脂血症等的高发,其患病率有明显增高的趋势[2]。目前对NAFLD的诊断主要依赖影像学检查[3],实验室诊断缺乏特异性指标,本研究对286例B超诊断为NAFLD患者进行了血液生化指标和肝纤维化指标的检测结果报告如下,探讨其在非酒精性肝病诊断中的意义。
1 对象和方法
1.1 研究对象
NAFLD患者来源于本院2001年至2005年每年的区干部健康体检符合脂肪肝的B超诊断标准并排除高血压、冠心病、糖尿病、病毒性肝炎及遗传性疾病,无嗜酒史,共286例,其中男156例,女130例,年龄23岁~75岁,平均(48±9.2)岁。根据B超结果将患者分为轻度、中度、重度3组,轻度组148例,中度86例,重度组52例。100例不嗜酒的健康人同样为本区干部体检健康者,肝、肾功能及心电图均正常排除高血压、糖尿病等病,既往无肝炎和神经系统疾病史,神经系统检查无阳性体征,其中男58例,女42例,年龄22岁~69岁,平均(46.6±8.6)岁。
1.2 标本收集
早晨空腹抽取NAFLD患者和正常体检者血液,分离血清,并立即检测。
1.3 实验方法
血液生化指标TG、TC、HDLc、ALT、AST、GGT和ALP采用美国贝克曼公司LX-20全自动生化分析仪检测试剂均购自贝克曼公司。肝纤维化指标PCⅢ、HA、CⅣ和LN采用放射免疫法检测试剂由上海海军医学研究所提供。实验操作严格按说明书进行每个样本每项指标均作3个平行检测。各项生化指标同时检测质控标本。
1.4 统计学处理
资料用±s表示,组间比较用t检验和F方差分析。
2 结果
2.1 NAFLD患者血清酶学指标的改变
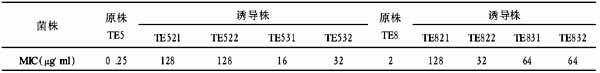
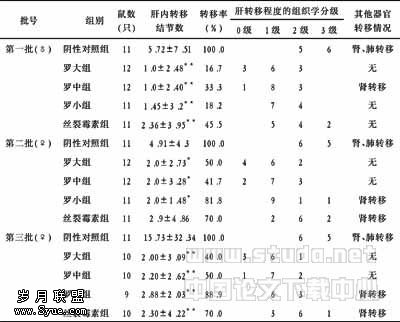
结果见表1。重度和中度脂肪肝组ALT、AST、GGT和ALP均明显升高(P<0.01) 但轻度组增高不显著(P>0.05)。表1 NAFLD患者血清酶学指标的改变(略)注:与正常人组比较*P<0.05;**P<0.01。
2.2 NAFLD患者血脂水平的改变
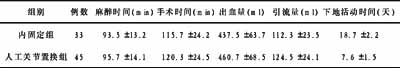
中度和重度非酒精性脂肪肝患者TG和TC水平均高于对照组,HDLc低于对照组,LDLc高于对照组;轻度非酒精性脂肪肝患者血脂水平与正常对照组比较差别无显著性。表2 NAFLD患者血脂水平的改变(略)注:与正常人组比较*P<0.05;**P<0.01。
2.3 NAFLD患者肝纤维化指标的改变
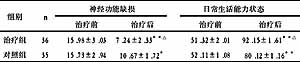
结果见表3。表3显示轻、中、重度NAFLD患者PCⅢ和HA均高于正常对照组;中、重度NAFLD患者CⅣ高于对照组;重度组LN高于对照组。表3 NAFLD患者肝纤维化指标的改变(略)注:与正常人组比较*P<0.05;**P<0.01。
3 讨论
NAFLD是一种全球性的疾病,累及世界范围内大量人群,虽然其患病率有一定的地理差异,在总人群中,NAFLD的患病率为20%(15%~39%),NASH的患病率为2%~3%。在日本NAFLD占非嗜酒者的14%,而在美国成人中NAFLD的患病率高达23%,是最常见的肝脏疾病[4]。我国对于NAFLD的大规模流行病学调查报告,北京报道的职员发病率为11.0%(116/1 050),上海为12.8%(513/4 009),杭州为5.2%(157/3 015)[5]。NAFLD可发生于任何年龄,包括儿童,多数研究报道好发于中年女性。NAFLD的危险因子包括肥胖、2型糖尿病、高血脂,均与胰岛素抵抗有关。NASH患者40%~100%有肥胖,21%~75%合并糖尿病,21%~83%合并高脂血症[6]。但是近年报道NASH 也发生于没有上述危险因子的患者。目前认为无症状性转氨酶升高、影像学提示脂肪肝和无法解释的持续性肝肿大患者应高度怀疑NAFLD。影像学检查如B超、CT、磁共振能发现肝内脂肪堆积,是目前诊断脂肪肝的有效手段,但在实验室诊断方面尚无特异性检测指标。本研究通过对286例NAFLD患者血液生化指标和肝纤维化指标进行检测发现NAFLD患者TG和TC水平均高于对照组(P<0.01),HDLc和LDLc与对照组相比分别呈下降和升高的趋势;重度NAFLD组ALT、AST和GGT明显升高(P<0.01),ALP升高不显著(P>0.05);NAFLD患者PCⅢ、HA、CⅣ和LN均高于健康组(P<0.05),重度组与轻、中度组之间PCⅢ、HA、CⅣ和LN差异均有显著性(P<0.01),中度脂肪肝与轻度脂肪肝之间PCⅢ、HA、CⅣ和LN差异无显著性(P>0.05)。提示NAFLD患者血清酶学指标和血脂指标均异常,并有不同程度的肝纤维化倾向,且随病情加重肝纤维化各项指标检测值升高越明显。已有报道NAFLD患者血清ALT升高最为常见,并常伴有AST升高,而且通常不超过正常上限的2倍~3倍,但血清转氨酶升高的程度与组织学表现无显著相关[7]。目前普遍认为,NASH是进展的,而单纯性脂肪变性和非特异性炎症可能并不会进展为肝纤维化和肝硬化,但NASH患者中大约37%~50%有肝纤维化。因此及时对NAFLD患者进行监测,对了解其病情,防止向NASH具有重要意义。分析我们的研究结果我们认为血液生化指标的检测可作为NAFLD筛查的重要依据,而肝纤维化指标的检测可进一步作为NAFLD病情监控和疗效评估的重要依据。
:
[1]Harrison SA,Kadakia S,Lang KA,et al.Nonalcoholic steatohepatitis:what we know in the new millennium[J].Am J Gastroenterol,2002,97:27142724.
[2]Schaffler A,Scholmerich J,Buchler C.Mechanisms of disease:adipocytokines and visceral adipose tissueemerging role in nonalcoholic fatty liver disease[J].Nat Clin Pract Gastroenterol Hepatol,2005,2(6):273280.
[3]Riley TR,Bruno MA.Sonographic measurement of the thickness of subcutaneous tissues in nonalcoholic fatty liver disease versus other chronic liver diseases[J].J Clin Ultrasound,2005,33(9):439441.
[4]Clark JM,Brancati FL,Diehl AM.Nonalcoholic fatty liver disease[J].Gastroenterology,2002,122:16491657.
[5]范建高.NAFLD的临床流行病学研究[J].消化杂志,2002,22:106107.
[6]Kumar KS,Malet PF.Nonalcoholic steatohepatitis[J].Mayo Clic Proc,2000,75:733739.
[7]Angulo P,Deach JC,Batts KP,et al.Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis[J].Hepatology,1999,30:13561362.