全麻诱导中地塞米松联合氟哌啶预防腹腔镜胆囊切除术后的恶心呕吐
【摘要】 目的:探讨全麻诱导中地塞米松联合氟哌啶预防腹腔镜胆囊切除术后恶心、呕吐的效果。方法:随机将240例ASAⅠ~Ⅱ腹腔镜胆囊切除术患者分为3组(各80例)。Ⅰ组(对照组)全麻诱导中不用地塞米松、氟哌啶;Ⅱ组全麻诱导中用地塞米松10mg;Ⅲ组全麻诱导中用地塞米松10mg和氟哌啶40μg/kg,观察术后48h患者的恶心、呕吐情况。结果:Ⅰ组患者恶心、呕吐的发生率为72.5%;Ⅱ、Ⅲ组恶心、呕吐的发生率分别为32.5%和7.5%,组间比较差异有统计学意义(P<0.05)。结论:全麻诱导中用地塞米松联合小剂量氟哌啶能预防腹腔镜胆囊切除术后的恶心、呕吐。
【关键词】 地塞米松 氟哌啶醇 恶心 呕吐 胆囊切除术 腹腔镜
The prevention of nausea and vomiting after laparoscopic cholecystectomy with dexamethasone combined with droperidol during induction of general anesthesia
【Abstract】Objective:To explore the effect of prevention for postoperative nausea and vomiting after laparoscopic chyolecystectomy with dexamethasone combined with droperidol during induction of general anesthesia.Methods:Two hundred and forty patients with ASA ⅠⅡ who would undergo laparoscopic cholecystectomy were randomly divided into three groups (80 patients in each group).Group Ⅰ(control group) was not given dexamethasone and droperidol in induction of general anesthesia.Group Ⅱ was given only 10 mg dexamethasone.Group Ⅲ was given 10 mg dexamethasone and 40 ug/kg droperidol.All patients were observed within postoperative 48 hours for nausea and vomiting.Results:The incidence of nausea and vomiting in group Ⅰ,Ⅱ and Ⅲ was respectively 72.5%,32.5% and 7.5%,which had significant differences among groups (P<0.05).Conclusions:The nausea and vomiting after laparoscopic cholecystectomy can be prevented maximally with dexamethasone combined with droperidol in small dose during induction of general anesthesia.
【Key words】Dexamethasone;Droperidol;Nausea;Vomitinging;Cholecystectomy,laparoscopic
患者在腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC)后易发生恶心、呕吐[1,2],全麻诱导中地塞米松对恶心、呕吐有预防作用,联合其他药物是否更加有效有待证实。我们探讨了地塞米松、氟哌啶对LC全麻诱导中防治恶心、呕吐的效果,现报道如下。
1 资料与方法
1.1 临床资料
择期LC患者240例,ASAⅠ~Ⅱ级,18~70岁,体重35~80kg。随机分成3组,每组80例。Ⅰ组为对照组;Ⅱ组为地塞米松组;Ⅲ组为地塞米松、氟哌啶组。有全身麻醉史,曾服用抗恶心、呕吐药的患者除外。
1.2 用药方法和监测指标
麻醉诱导中,Ⅰ组依次静注依托咪酯0.3mg/kg、芬太尼4~6μg/kg、维库溴胺0.12mg/kg;Ⅱ组比Ⅰ组另加地塞米松10mg;Ⅲ组比Ⅱ组另加氟哌啶40μg/kg。麻醉维持系间歇静注芬太尼,用维库溴胺维持肌松和吸入氨氟醚。术毕常规用新斯的明0.5mg,阿托品0.5mg,拮抗残余肌松作用,术中连续监测患者的血压(MAP)、氧饱和度(SpO2)、心率(HR)、气腹压等。
1.3 术后观察指标
从术毕开始持续到术后48h记录3组患者恶心、呕吐(包括干呕)次数以及焦虑、不安、失眠等副作用,并统计患者术后的住院时间。
1.4 统计学处理
计量资料与计数资料分别用t检验和χ2检验,P<0.05为差异有统计学意义。
2 结 果
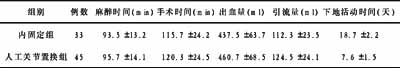
3组患者在ASA分级、年龄、性别、体重、麻醉时间、手术时间、CO2气腹压力及等方面均无统计学差异(P>0.05)。术后48h,3组患者恶心、呕吐的发生率组间差异有统计学意义(P<0.05)。见表1。3组患者均未出现明显的焦虑、不安、失眠等副作用及并发症,术后住院天数分别为4.0d、4.2d、4.1d,无统计学差异(P>0.05)。表13组患者术后48h的恶心、呕吐情况(略)
3 讨 论
恶心呕吐是麻醉和手术后较常见的并发症,会使患者感到不安和痛苦,甚至引起切口裂开,电解质紊乱,营养缺乏,增加了住院时间及费用。严重的恶心呕吐、术后疼痛和术中知晓已成为患者术后不愉快的3个因素[3]。因而,有效预防和减少恶心呕吐有重要的临床意义。
不同手术恶心呕吐的发生率不相同,本资料中对照组术后恶心呕吐发生率为72.5%,2个实验组恶心、呕吐的发生率则明显降低,尤以地塞米松、氟哌啶组最为显著,表明地塞米松能降低LC术后恶心呕吐的发生,加用氟哌啶则效果更好。
从生理角度讲,引起恶心呕吐的机理尚未完全清楚,但与多巴胺和5?羟色胺(5?HT)受体的关系密切[4],LC手术还与CO2气腹,腹腔操作刺激胃或损伤胃粘膜及应用的麻醉药物、术后疼痛和镇痛等药物的应用以及性别等因素有关[5],各种不良因素通过多种神经递质刺激外周感受器和呕吐中枢引起恶心呕吐[6]。鉴于并非单一因素引起恶心呕吐,提示联合使用抗恶心呕吐药物比单一用药更加有效。
地塞米松是常用药,具有多种药理作用,但其抗恶心呕吐的机理尚不完全清楚,可能包括抑制前列腺素合成,使中枢神经系统5?HT生成减少,以及改变血脑屏障对血清蛋白的通透性,降低了血液中5?HT作用于大脑后极区化学催吐感受区的浓度。氟哌啶是多巴胺受体拮抗剂,也是5?HT受体拮抗剂。α1受体和较弱的α2受体激动剂,其止吐作用是通过以上多种机制实现的[7]。
综上所述,地塞米松联合小剂量氟派啶能有效预防LC术后恶心呕吐的发生,且无明显的副作用。
【】
[1]Liu K,Hsu CC,Chia YY.Effect of dexamethasone on postoperative emesis and pain[J].Br J Anaesth,2003,90(2):254?256.
[2]Rothenberg DM,Peng CC,Normoyle DA.Dexamethasone minimizes postoperative nausea and vomiting in at patients[J].Anesth Analg,1996,82(suppl):S388.
[3]Myles PS,Williams DL,Hendrata M,et al.Patient satisfaction after anaesthesia and surgery:results of a prospective survey of 10 811 patients[J].Br J Anaesth,2000,84(1):6?10.
[4]Wang JJ,Ho ST,Liu YH,et al.Dexamethasone reduces nausea and vomiting after laparoscopic cholecystectomy[J].Br J Anaesth,1999,83(5):772?757.
[5]Mehernoor F,Watcha MD,Paul F,et al.Postoperative nausea and vomiting[J].Anesthesiology,1992,77(1):162?184.
[6]Kovac AL.Prevention and treatment of postoperative nausea and vomiting[J].Drugs,2000,59(2):213?243.
[7]Naj I,P' Farschtschian M,Wilder?smith OH,et al.Epidural droperidol and morphine for postoperative pain[J].Anesth Analg,1990,70(6):583?588.