Immune modulation by parenteral lipid emulsions
作者:Geert JA Wanten and Philip C Calder,
【摘要】 Total parenteral nutrition is the final option for nutritional support of patients with severe intestinal failure. Lipid emulsions constitute the main source of fuel calories and fatty acids (FAs) in parenteral nutrition formulations. However, adverse effects on patient outcomes have been attributed to the use of lipids, mostly in relation to impaired immune defenses and altered inflammatory responses. Over the years, this issue has remained in the limelight, also because technical advances have provided no safeguard against the most daunting problems, ie, infectious complications. Nevertheless, numerous investigations have failed to produce a clear picture of the immunologic characteristics of the most commonly used soybean oilCderived lipid emulsions, although their high content of nC6 polyunsaturated FAs (PUFAs) has been considered a drawback because of their proinflammatory potential. This concern initiated the development of emulsions in which part of the nC6 FA component is replaced by less bioactive FAs, such as coconut oil (rich in medium-chain saturated FAs) or olive oil (rich in the nC9 monounsaturated FA oleic acid). Another approach has been to use fish oil (rich in nC3 PUFA), the FAs of which have biological activities different from those of nC6 PUFAs. Recent studies on the modulation of host defenses and inflammation by fish-oil emulsions have yielded consistent data, which indicate that these emulsions may provide a tool to beneficially alter the course of immune-mediated conditions. Although most of these lipids have not yet become available on the US market, this review synthesizes available information on immunologic characteristics of the different lipids that currently can be applied via parenteral nutrition support.
【关键词】 total parenteral nutrition lipid emulsion immunology inflammation fatty acids eicosanoids
INTRODUCTION
Over the past 4 decades, parenteral nutrition has proven itself to be the therapeutic strategy of choice for nutritional support of patients with severe chronic intestinal failure (1). Total parenteral nutrition (TPN) implies that all macronutrient (carbohydrates, amino acids, and lipids) and micronutrient (electrolytes, vitamins, and trace elements) requirements are met by means of an 'all-in-one' sterile, aqueous solution that is administered into a large-bore central vein (2). Although nontunneled catheters positioned in the subclavian or jugular veins can be used for short-term TPN delivery in hospitalized patients, long-term TPN administration in the home setting requires the presence of a tunneled catheter, a subcutaneous port, or an arteriovenous shunt to provide a site for venous access (3). Although the relevance of TPN support for clinical practice is beyond doubt, its high rate of complications remains a drawback (4). The nature, magnitude, and suggested management of these complications have been addressed (1, 5). Although mechanical (catheter occlusion) and metabolic (disturbances of fluids and electrolytes, liver dysfunction, and bone disease) problems frequently occur, complications related to venous access and infection remain the major problems (4, 6). With respect to the latter, lipids in TPN formulations have long been under scrutiny because of their alleged detrimental effects on immune function. For instance, a meta-analysis in surgical and critically ill patients reported higher complication rates in patients receiving lipid-based TPN than in those receiving lipid-free formulations (7). However, the overall clinical proof for such negative effects is rather weak (8). Also, novel lipids have recently been introduced in the clinical arena, which promise to modulate inflammatory responses in a favorable manner and to improve the outcomes of patients with immune-mediated conditions. These notions provided the background for the present review, which provides an overview of and insights regarding the currently available data on immune modulation by parenteral lipids.
HISTORICAL PERSPECTIVE
Lipids, in the form of olive oil (OO) and milk, for example, have been administered intravenously to humans for therapeutic purposes since the 17th century (9). Numerous adverse events resulting from lipid use led to the notion that the administration of fat by this route invariably causes severe complications, including fat embolism. The demonstration of a strong link between the presence of malnutrition and the development of postoperative mortality in the 1930s by Studley (10) was a strong impetus for the exploration of better ways to deliver adequate fuel calories to these patients. After much trial and error, Schuberth and Wretlind (11) eventually succeeded in developing a nontoxic lipid emulsion prepared from soybean oil (SO) (Intralipid; Fresenius-Kabi, Bad Homburg, Germany) that was introduced in 1961. Wretlind's system of lipid-based TPN found its way into Europe during the 1960s and 1970s (12-14). By contrast, high-osmolar glucose solutions, based on Dudrick's concept of hyperalimentation, remained the sole intravenous nonprotein energy supply for patients in the United States, where lipid emulsions had as yet not been accepted (15, 16). This changed when the glucose system was found to cause serious side effects, including hyperglycemia, liver steatosis, and deficiencies of fatty acids (FAs) and fat-soluble vitamins, whereas lipid infusion was shown to prevent fatty infiltration of the liver and to minimize metabolic stress (9, 17).
PARENTERAL LIPID EMULSIONS: COMPOSITION AND METABOLISM
Lipids are an energy-dense source of fuel calories (9 kcal/g) compared with proteins and carbohydrates (both 4 kcal/g). It is generally recommended in clinical practice that the lipid supply should provide 15C30% of the total calorie intake, or 30C50% of nonprotein calories (18). Infusion of parenteral lipid emulsions at rates of 0.8C1.5 g/kg body wt per day is safe but should not exceed 2.6 g/kg per day (0.11 g/kg per hour), because side effects have been reported above this threshold (19). Especially in metabolically stressed patients, the safest way to administer parenteral lipids is by continuous infusion at the lowest possible rate, because the discontinuous administration with condensing of daily dosages promotes the development of problems related to fat overload, such as hypertriglyceridemia, liver- and respiratory dysfunction, and coagulopathy (18, 20-22).
Lipid emulsions for parenteral use are provided at triacylglycerol concentrations of 10%, 20%, or 30% (wt:vol). These emulsions are isoosmotic (mean pH: 7.5), whereas TPN formulations as a whole are hypertonic (pH: 6.0) (22). Lipid emulsions consist of 100C500-nm droplets to simulate chylomicrons, the lipoproteins that transport dietary FAs in circulating blood, with a monolayer of phospholipids enveloping a triacylglycerol core (23). The phospholipids act as an emulsifier and are usually derived from egg yolk. The emulsions also contain other lipid-soluble substances, such as vitamins E and K, lipid peroxidation products, and phytosterols (24). Emulsion metabolism, similar to that of chylomicrons, is enhanced by the acquisition of apoproteins, mainly types C and E, which are transferred from HDLs and cover the lipid droplets very rapidly on infusion. The degradation of emulsion droplets takes place at endothelial sites of extrahepatic tissues by lipoprotein lipaseCmediated hydrolysis, which results in FA release and a reduction in size of the emulsion remnant particles (23, 25). Hormonal (eg, insulin) and cytokine balance and lipid composition regulate this process. The final step in the intravascular emulsion degradation process involves tissue uptake of remnant particles in the liver, which results in the intracellular delivery of fat-soluble vitamins and FAs that have not been released by lipoprotein-lipase-mediated hydrolysis. A nonspecific hepatic lipase that hydrolyzes triacylglycerols, mono- and diglycerides, cholesteryl esters, and phospholipids controls this process (26). Lipid emulsions contain more phospholipids than necessary to solubilize their triacylglycerol content. Emulsions containing 10% lipids have an especially high ratio of phospholipids to triacylglycerols, greater than that of 20% emulsions and even more than 30% emulsions. Part of this is present as 80C100 nm liposome-resembling particles that impede lipid metabolism and accumulate as an abnormal lipoprotein X, which leads to hypercholesterolemia. It is therefore recommended that lipid emulsions be administered at higher concentrations and at a low speed to prevent liposome accumulation (23, 24, 27).
Bioactive emulsion components other than lipids
Lipid emulsions are prepared from biological materials that may differ between batches in their content of bioactive substances, such as antioxidants (eg, various tocopherol isoforms) (28). Polyunsaturated FAs (PUFAs) in lipid emulsions, depending on the degree of protection by antioxidants and under the influence of various storage conditions (eg, light exposure and temperature), can peroxidize to potentially harmful lipid hydroperoxides (29, 30). The discussion on the immunologic effects of these substances is beyond the scope of this article and will not be considered further.
STRUCTURALLY DIFFERENT FATTY ACIDS AND LIPIDS IN TPN
Structure of lipids and fatty acids
Lipids supply most of the nonglucose fuel calories and they are building blocks for cellular components and essential FAs. Lipids in TPN formulations are triacylglycerols consisting of 3 FAs attached to a glycerol backbone. FAs are hydrocarbon chains with a methyl group at one end of the chain and a reactive carboxyl group at the other end (Figure 1). In most biological systems, the chain length of the component FAs varies from 2 to 30 carbons. FA and their corresponding triacylglycerols can be classified as short chain (up to 4 carbons), medium chain (MCFA or MCT; 6C12 carbons), or long chain (LCFA or LCT; 14 carbons) (31). Double bonds can be inserted into the hydrocarbon chain, and FAs can also be classified based on the number of double bonds present. A saturated FA has no double bonds in the hydrocarbon chain, whereas monounsaturated FAs (MUFAs) and polyunsaturated FAs (PUFAs) have 1 or 2 or more double bonds, respectively (Figure 2). The final means of classification of FAs is the position of the double bonds within the hydrocarbon chain. This is what gives rise to the nC or nomenclature for FAs. The 3 principal families of unsaturated FAs are the nC9, nC6, and nC3 families. This means of classification indicates the carbon on which the first double bond occurs when counting from the methyl carbon of the hydrocarbon chain. The simplest nC6 and nC3 PUFAs are linoleic acid (18:2nC6) and -linolenic acid (18:3nC3), respectively (Figure 2).
FIGURE 1. Generic structure of a fatty acid.
FIGURE 2. Structure and naming of selected 18-carbon fatty acids.
In humans, linoleic and -linolenic acids are termed essential FAs because their de novo synthesis is not possible and availability, therefore, completely depends on the diet (32). These FAs are synthesized in plants; therefore, plant tissues, seeds, and seed oils tend to be good sources of essential FAs. Although linoleic and -linolenic acids cannot be synthesized in humans, both FAs can be elongated and desaturated by mammalian enzymes, principally in the liver. This pathway of metabolism is shown in Figure 3, which indicates the direct competition for metabolism between the 2 families of PUFAs. Metabolism of linoleic acid yields arachidonic acid (AA, 20:4nC6) as the major end product, while eicosapentaenoic (EPA, 20:5nC3) and docosahexaenoic acid (DHA, 22:6nC3) are end products of the metabolism of -linolenic acid. Although -linolenic acid is the preferred substrate for the 6-desaturase enzyme, on most typical Western diets the metabolism of linoleic acid is quantitatively more important because the diet contains 5 to 20 times more linoleic than -linolenic acid. Thus, blood and cell lipids typically contain much more AA than do very-long-chain nC3 PUFAs. The only rich dietary source of very-long-chain nC3 PUFAs is seafood, especially fatty fish such as salmon, herring, and mackerel. These FAs are also found in commercial products termed fish oils (FOs). Just as there is competition for metabolism between linoleic and -linolenic acids, there is competition between AA and EPA for incorporation into cell membranes and for metabolism to bioactive eicosanoid mediators.
FIGURE 3. Synthesis of long-chain nC6 and nC3 polyunsaturated fatty acids from their precursors.
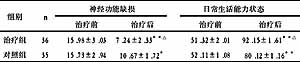
MECHANISMS INVOLVED IN IMMUNE MODULATION BY PARENTERAL LIPIDS
FAs are key determinants of the structural integrity of cell membranes. FA structure, especially chain length and degree of unsaturation, is critical to the interaction of lipids with immune cells (33). Exposure to lipids with different FA compositions may influence immune cells through several features relating to cell membrane structure and function that are highly interactive (Figure 4) (34-36).
FIGURE 4. Mechanisms by which fatty acids can affect immune cell function. NF-B, nuclear factor B.
Membrane fluidity
This refers to a complex property involving the mobility of membrane components and permeability characteristics, with a key role in enzyme and surface receptor functions. FAs have been shown to affect lymphocyte membrane fluidity in a structure-dependent manner (37). Effects of parenteral lipids on membrane fluidity have been shown in vitro and were found to depend on FA structure (38). MCT, and, to a lesser extent, MCFA-containing structured lipids (SLs), increase the membrane fluidity of isolated neutrophils, whereas an SO-based LCT emulsion, rich in the nC6 PUFA linoleic acid, exert no effect. Within the cell membrane, phospholipid bilayer microdomains exist, so-called lipid rafts, with a unique lipid environment that facilitates intercellular signaling and cross talk. Many receptors and signaling proteins are localized in such rafts (39). Although one study has reported that infusion of an SO-based emulsion rich in nC6 PUFAs alters lipid raft organization and decreases the membrane fluidity of human T cells, others found that pure nC3 PUFAs displace acylated proteins from rafts in these cells and thus alter cell function (40, 41). Other than these sparse data, data concerning the effects of parenteral lipids on the distribution and composition of lipid rafts in immune cells are unavailable.
Production of bioactive mediators
AA, EPA, and DHA all give rise to bioactive lipid mediators. The best characterized of these are the eicosanoids produced from AA: prostaglandins, thromboxanes, and leukotrienes. Before synthesis of these mediators, the parent FA (ie, AA, EPA, or DHA) is released from these cell membrane phospholipids by the action of phospholipase A2. The subsequent metabolism of AA by cyclooxygenase enzymes yields the 2-series prostaglandins and thromboxanes, whereas the metabolism by 5-lipoxygenase yields the 4-series leukotrienes. In general, these mediators have pro-inflammatory actions (42, 43). EPA also acts as a substrate for cyclooxygenase and lipoxygenase, giving rise to 3-series prostaglandins and thromboxanes and 5-series leukotrienes. The functional significance of this is that the products formed from EPA are typically less potent than are those formed from AA. Increased provision of EPA results in partial replacement of AA in cell membrane phospholipids, with a resulting decrease in capacity to produce the AA-derived eicosanoids and an increased capacity to produce those from EPA. In addition to very-long-chain nC3 PUFAs modulating the generation of eicosanoids from AA and to EPA acting as substrate for the generation of alternative eicosanoids, recent studies have identified a novel group of protective mediators, termed E- and D-series resolvins, formed from EPA and DHA, respectively, that dampen acute leukocyte responses and facilitate the resolution of inflammation (44, 45). These substances may well underlie at least some of the beneficial actions of nC3 PUFAs, especially in chronic disorders in which unresolved inflammation is a key mechanism of pathogenesis (46).
Cell signaling
Lipid-induced changes in membrane composition alter properties of phospholipid-derived second messengers involved in cell signal transduction (47, 48). Indeed, parenteral lipids have been found to influence Ca2+- and protein kinase CCmediated signaling of activated neutrophils, depending on their structure (49, 50). Specifically, MCT-containing emulsions, but not SO-based LCTs, mimic the potent protein kinase CCactivating phorbol ester phorbol myristyl acetate (PMA) by markedly increasing the rise in intracellular Ca2+ concentrations that are brought about by opsonized particles, as a mimic for invading microorganisms. MCT, similar to PMA, also evoke a leftward shift of the dose-response curve for these Ca2+-concentration rises, suggesting protein kinase CCdependent sensitization of neutrophils for stimulation (49). Of note, this MCT-related phenomenon was not observed with MCFA-containing SLs.
Saturated FAs and PUFAs differentially regulate pathways involved in the coordination of innate and acquired immune responses. The former involves the action of so-called Toll-like receptors (TLRs), which signal the presence of invading microbes by recognizing conserved pathogen-associated molecular patterns (51). For example, TLR-4 is the receptor for microbial lipopolysaccharide. Although saturated FAs activate TLR-4Cmediated pro-inflammatory pathways, with stimulation of nuclear transcription factor B and expression of cyclooxygenase-2, these events are inhibited by very-long-chain nC3 PUFAs (52, 53). Thus, differential TLR subtype stimulation may bring specificity to innate immunity (54).
Regulation of gene expression
FAs can affect cell responses through the regulation of gene expression and subsequent downstream events by acting as ligands for nuclear receptors. For instance, very-long-chain nC3 PUFAs control transcription factors such as peroxisome proliferatorCactivated receptors (PPARs) and sterol-regulatory-element binding proteins (55). PPARs can bind to DNA and are involved in the regulation of inflammatory processes, lipid metabolism, and energy utilization by modulating the expression of target genes, for instance by repressing signaling through nuclear transcription factor B (35, 55). Because FAs influence many genes, their effects on cellular responses vary widely, ranging from changes in surface adhesion molecule expression to altered cytokine production.
Modulation of apoptotic pathways
Infusion of SO-based LCTs in humans has been found to increase the apoptotic rate of cultured lymphocytes, whereas cell necrosis was not influenced (40). Because of its design, this study could not determine whether this is a lipid-specific effect. FAs seem to promote in vitro apoptosis and necrosis in lymphocytes, with the parent nC6 PUFA linoleic acid acting on mitochondrial depolarization and oxygen radical production, whereas the nC9 MUFA oleic acid is less toxic and affects the activation of caspase 3 (56). Invading microorganisms, depending on their nature, trigger specific human immune responses that involve the differentiation of T helper type 0 lymphocytes (Th0) into type 1 (Th1) cells that are involved in phagocyte activation and antibody-dependent cellular cytotoxicity, whereas type 2 (Th2) cells mainly act against parasitic infections. When compared with nC6 PUFAs, nC3 PUFAs enhance the activation-induced cell death of Th1 cells, but leave Th2 cell apoptosis unaffected (57). This suggests that nC3 PUFAs modulate T cellCmediated immunity by selective deletion of Th1-like cells while maintaining Th2-mediated responses.
Effects on other immune-modulating substances
FAs may also exert effects through their influence on the metabolism of other compounds that are involved in the regulation of immune responses. For instance, eicosanoids derived from AA increase the expression of the arginase I enzyme and thus may decrease the amount of available arginine, whereas eicosanoids from EPA have the opposite effect (58).
IMMUNOLOGIC EFFECTS OF STRUCTURALLY DIFFERENT PARENTERAL LIPIDS
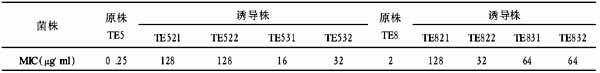
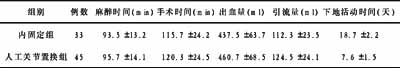
It is generally accepted that a lipid emulsion in its ideal form should be easily accessible for metabolic breakdown, but should not confer any inflammatory or oxidative stress or impair the function of the immune system (8). On the basis of these notions, several lipid emulsions have been developed over the years. Relevant information regarding some of these emulsions is presented in Tables 1 and 2.
TABLE 1 Characteristics of commercial lipid emulsions according to the manufacturers1
TABLE 2 Fatty acid composition of lipid emulsions1
SO-based lipid emulsions
Parenteral LCT, derived from SO or safflower oil, such as Intralipid and Ivelip (Baxter, Maurepas, France), have a high ratio of nC6 to nC3 PUFAs (7:1) because of their high content of linoleic acid and only moderate amounts of -linolenic acid (Table 1). This has been considered a drawback that might promote the overproduction of pro-inflammatory eicosanoids and increase oxidative stress in clinical situations (eg, sepsis and trauma) that are already dominated by imbalanced immune responses (59, 60).
With reference to clinical outcome, concerns regarding detrimental effects of parenteral SO on immune function were raised by early clinical observations in the 1980s that showed an increased risk of bacteremia in neonatal patients using lipid-based TPN (61-63). Snydman et al (64) observed that intravenous lipids increased infection rates in surgical patients and were the first to propose the lipid-induced promotion of bacterial growth in intravenous lines as an underlying mechanism. Lipid-induced immune suppression was also suggested in clinical studies that found an increased risk of infectious complications in mildly malnourished surgical patients and lower rates of graft versus host disease after bone marrow transplantation in patients using SO-based TPN (65, 66). On the other hand, a large randomized clinical trial in 482 patients undergoing bone marrow transplantation found no evidence of a role of Liposyn II (Abbott Laboratories, North Chicago, IL), a safflower-based emulsion, on the incidence of bacteremia or fungemia when patients were assigned to receive either 6C8% (the low-dose group) or 25C30% (the standard-dose group) of total daily energy as a 20% lipid emulsion (67).
Understandably, these conflicting clinical reports evoked a flood of experimental work aiming to characterize lipid effects on immune functions and provide pathophysiologic explanations for these lipid effects. Some studies indeed showed SO-induced impairments in phagocyte functions, such as granulocyte migration and phagocytosis, in vitro and ex vivo (68-71). Importantly however, these investigations used lipids at supraphysiologic concentrations up to 100 mg/mL, or 115 mmol/L (ie, a dose well above the upper threshold of 10 mmol/L that can be considered clinically relevant) (68-70). Also, the study by Fisher et al (71) and that by Palmblad (72) were criticized because of its nonphysiologic model, wherein lipids and streptococci were injected intraperitoneally in mice. SO-induced impairments in the function of the hepatic reticuloendothelial system (RES), and interference with lipopolysaccharide-induced cell stimulation, as was observed with HDLs, have been proposed as underlying mechanisms to explain the immunosuppressive effects of intravenous lipids (73, 74). However, the overall data regarding the effects of SO on immune responses have been disparate, because many investigators in numerous clinical and experimental settings found no evidence of an effect on a wide range of features and functions of various immune cells, cellular signal transduction, or membrane characteristics (35, 74-83). Of note, these latter investigators, with the exception of some (81, 82), used lipids in a clinically relevant concentration range. Taken together, different experimental approaches in animal and human studies most probably play an important role in the ongoing controversy (77).
Physical mixtures of SO and medium-chain triacylglycerols
Saturated MCTs, present in coconut and palm kernel oils, have traditionally been regarded to be good sources of fuel calories but to have with few other physiologic roles. Compared with SO, MCTs have biochemical properties that render them a superior source of energy in clinical situations of depletion, because of their easy accessibility for metabolic degradation (84). Compared with LCFAs, MCFAs are 100 times more soluble in water and can directly pass into cells without binding to FAs or transport proteins. Also, -oxidation of MCFAs, in contrast with that of LCFAs, does not require carnitine for transport into mitochondria and also takes place in peroxisomes (85-87). Whereas LCFAs are incorporated into chylomicrons after absorption from the intestine and eventually reach the systemic circulation via the lymph system, MCFAs, on absorption, are directly transported to the liver via the portal vein (85).
In the mid-1980s, physical mixtures containing SO and MCTs, such as Lipofundin (B Braun, Melsungen, Germany), became available for TPN practice, reflecting the wish to decrease the high content of nC6 PUFAs in lipid emulsions. Besides their rapid metabolic breakdown, MCts were also chosen because of their resistance to peroxidation (88, 89). The use of LCTs, however, remained necessary because humans do not tolerate pure MCTs, and MCTs are not a source of essential FAs. The special qualities of MCTs offer both benefits and risks, ie, positive effects on protein metabolism and on RES function but an increased risk of ketogenesis and acidosis (90, 91). Also important, the mix of SO and MCTs decreases glucose oxidation to a lesser extent than does pure SO (92). This finding is especially relevant because insulin resistance and hyperglycemia play a crucial role in the development of complications during critical illness (93). Glucose has also been found to decrease the oxidation of LCFAs, such as oleic acid, but not of MCFAs, such as octanoic acid, by affecting FA entry into mitochondria (94).
MCT-containing emulsions are not yet commercially available in the United States, despite their proven tolerability and rapid clearance in severely ill malnourished patients (90, 95-99). Of note, these data come from small (20 patients) short-term (10 d of lipid administration) studies that were not designed to evaluate clinical endpoints such as infectious complications and patient survival. One larger study, by Garnacho-Montero et al (99), included 72 septic patients, but it has only been published in Spanish. The only larger prospective randomized trial to report on a clinical endpoint (infectious complications), by Grau et al (100), was a short-term (5 d of lipid administration) study that has only been published in Spanish. These investigators compared SO-MCTs and SO given for 2 d preoperatively and 3 d postoperatively to 72 severely malnourished patients who underwent a laparotomy because of suspected malignancy (100). Overall, it was found that SO-MCTs significantly reduced the incidence of intraabdominal abscesses when compared with SO-based TPN, without an effect on other infections. In addition, in the subgroup of patients without cancer, SO-MCTs decreased mortality (100).
With respect to the mechanisms behind the effects of MCTs on outcome, it has been shown that infusion of SO-MCTs impairs lung function and aggravates tissue inflammation in patients with acute respiratory distress syndrome, but not in healthy subjects (101). On the other hand, this might also represent a nonspecific lipid effect, as was suggested by the finding that pure SO induced similar abnormalities (102). As with SO, and probably because of similar flaws in experimental design, numerous investigations have failed to produce a uniform picture of the immunologic effects of SO-MCTs (103). In the experimental setting, when compared with other lipids, MCTs at clinically relevant concentrations up to 5 mmol/L, increase 2-integrinCmediated human phagocyte adhesion and cell membrane fluidity but decrease motility and the capacity of these cells to kill fungal pathogens (104-107). MCFAs also increase the expression of PPAR- and other transcription factors in adipocytes (108). In addition, SO-MCTs and pure MCTs distinctly modulate calcium- and protein kinase CCmediated cell signaling of human neutrophils (49, 50). Taken together, these findings suggest that MCTs activate isolated immune cells, but at the same time impair several cell functions. Also important, these data challenge the view that immunologic effects of lipids are essentially determined by their ratio of nC6 to nC3 PUFAs because SO-MCTs and pure SO are equivalent in this respect (109). The relevance of these findings in clinical practice, however, remains to be established.
Structured lipids
The considerations on metabolism and immunology regarding SO and MCTs in the 1990s resulted in the development of synthetic SLs, such as contained in Structolipid (Fresenius-Kabi). These SL are made by hydrolysis of SO and MCTs with subsequent random reesterification of MCFAs and LCFAs in the 1, 2, or 3 positions to glycerol (110-112). The type of core material influences the circulation time of lipids, because emulsions with MCFAs in the 1,3 position are removed more slowly from the circulation than are those with LCFAs in these positions (112).
No long-term clinical trials have yet been conducted that have evaluated SL effects on infectious complications and patient survival, although data from several short-term investigations suggest that SLs are well tolerated and are more rapidly oxidized and cleared from the plasma when compared with SO and SO-MCTs (22, 110, 113). Studies in humans and animals indicate that the use of SLs in catabolic subjects improves nitrogen balance, preserves the function of the RES, and disturbs liver function to a lesser extent than do SO and SO-MCTs (114, 115).
Only few data are available regarding the immunologic characteristics of SLs. Experimental work indicates that SL exposure at concentrations up to 5 mmol/L does not significantly influence phagocyte functions or cell signaling (49, 104, 106, 107). This is intriguing, given the presence of MCFAs in these triacylglycerols and the significant effects of MCTs on leukocyte function (see'Soybean oilCbased lipid emulsions' above). The preferential localization of MCTs at the surface of lipid droplets in physical SO-MCT mixtures is probably crucial, because MCFAs in SLs are evenly distributed within the lipid droplets (22). Finally, SLs and SO have shown beneficial effects on liver morphology in TPN-induced hepatosteatosis in rodents, with fewer fatty changes when compared with lipid-free or MCT-based formulations (116).
OO-based lipid emulsions
In the OO-based emulsion (Clinoleic; Baxter) that became available for use in TPN in the late 1990s, 80% of SO has been replaced by OO, which is rich in the long-chain nC9 MUFA oleic acid (18:1nC9). This results in MUFA and PUFA contents of 65% and 20%, respectively, with an nC6 to nC3 PUFA ratio of 9:1 (117).
The few small, short-term clinical trials that have been performed with OO should merely be considered as safety and tolerance studies that provide no insight into the immune-modulating effects of OO-based emulsions. A randomized double-blind trial in 19 children, with an SO emulsion as control, showed that prolonged (60 d) administration of OO was well tolerated and decreased the accumulation of toxic lipid peroxidation products (118). The safe use of OO, with beneficial effects on TPN-induced liver dysfunction and no side effects or altered inflammatory markers, has been confirmed in several small (14 subjects) studies in stable home TPN patients (117, 119, 120). Accordingly, a recent trial that unfortunately included a control group that received a lower dose of a different lipid (SO-MCT), reported good tolerance and an absence of side effects from OO-based TPN in 33 critically ill trauma patients (121).
Previous research has shed some light on the immunologic properties of OO. An increase in the dietary intake of oleic acid by healthy volunteers for 2 mo was found to decrease the expression of adhesion molecules of human mononuclear cells without affecting lymphocyte proliferation and natural killer cell activity (122). Similar immune-neutral effects have been observed with parenteral OO, eg, in an in vitro study that compared OO with 2 SO emulsions. Although both the latter suppressed lymphocyte proliferation and the production of interleukin (IL)-2, OO showed no deleterious effects (123). When the effects of lipid emulsions at concentrations up to 2.5 mmol/L on calcium signaling in human neutrophils were studied, it was found that all evoked a prompt attenuation of the cell stimulation by a bacterial tripeptide. However, OO and SO were by far less potent in this respect when compared with SO-MCT and FO (50). Olive oil has also been found to inhibit the production of proinflammatory cytokines by isolated human mononuclear cells at concentrations up to 1% (10 mmol/L), significantly less than SO and SO-MCT (124). Similarly, the expression of activation markers (CD11b, CD66b) on human neutrophils and mononuclear cells in whole blood did not change after exposure to OO at a concentration of 5 mmol/L, whereas SO-MCT elicited cell activation as evidenced by a significantly increased marker expression (105). Another recent study in this field also reported less of an effect of OO at concentrations from 0.03 to 3 mmol/L on human neutrophil functions (oxidative burst, chemotaxis, and elastase release) in vitro and on rat neutrophil adhesion ex vivo than of SO and SO-MCT (125). Two in vivo animal studies in rats are available to corroborate the immune-neutral effects of OO on leukocyte functions (spleen lymphocyte proliferation, IL-2 receptor expression, and bacterial clearance) in comparison with the deleterious effects observed for SO and SO-MCT (126, 127). Finally, somewhat more circumstantial evidence of an immune-neutral effect of OO is provided by a recent study that showed no evidence of oxidative damage or altered oxidant-antioxidant balances in a considerable portion (40%) of the Dutch home TPN population, most of whom (75%) were using an OO-based TPN formulation (128). In conclusion, there is not much evidence that OO directly influences immune function, although indirect effects may result from competition for incorporation with nC6 and nC3 PUFA into membrane phospholipids (35).
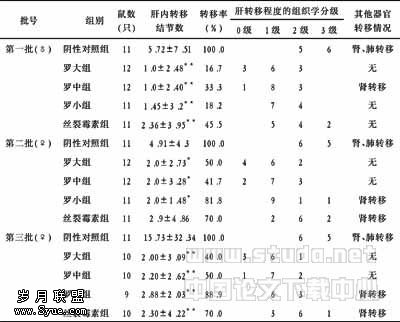
FO-based lipid emulsions
There is currently one emulsion available for parenteral use that contains FO as the single lipid source (Omegaven; Fresenius-Kabi). This 10% emulsion contains 100 g lipid/L, of which 27C59 g is EPA plus DHA, and has a very low ratio (1:8) of nC6 to nC3 PUFAs (Table 1). It is recommended to combine this fish-oil emulsion with others (eg, SO or SO-MCT) in such a manner that FO contributes 10C20% of infused emulsion. Another emulsion that includes FO is Lipoplus (B Braun), also known as Lipidm in some countries. This is a 20% lipid emulsion with the lipid being a mix of 50% MCT, 40% SO, and 10% FO. Each liter of Lipoplus contains 9C17 g EPA plus DHA. Studies in animal models show that inclusion of nC3 PUFAs in mixed lipid emulsions increases blood clearance and extrahepatic tissue uptake of lipid, despite the fact that FO is a poor substrate for lipoprotein lipase (89, 129, 130).
With regard to effects on outcome in animal studies, FO has been shown to improve survival in models of endotoxemia (131-135). FO also decreased endotoxin-induced metabolic perturbations in guinea pigs and rats and improved heart and lung function and decreased lung edema in endotoxic rats and pigs (134, 136-143). Compared with linoleic acidCrich vegetable oils, FO fed to rats before exposure to live bacteria (either as a result of cecal ligation and puncture or intravenous administration of live Group B Streptococcus, respectively) resulted in increased survival, which was associated with decreased production of prostaglandin E2 (144, 145). Infusion of FO after induction of sepsis by cecal ligation and puncture decreased mortality (and prostaglandin E2 production) compared with vegetable oil (146). Intragastric administration of FO into chow-fed rats before cecal ligation and puncture improved survival more than did saline or vegetable oil infusion (147).
At least one aspect of the pathophysiologic background behind these effects of FO on outcome appears to be an altered production of bioactive mediators in the form of diminished circulating concentrations of inflammatory eicosanoids (131-135, 144, 145). Feeding FO to mice decreased the ex vivo production of TNF-, IL-1, and IL-6 by endotoxin-stimulated macrophages (148-150). Several studies in healthy human volunteers involving supplementation of the diet with FO also have shown a decreased production of TNF-, IL-1, and IL-6 by endotoxin-stimulated monocytes or mononuclear cells (151-156). Besides the effects on eicosanoid and cytokine production, another important aspect of FO may be its positive effect of FO on bacterial killing by the host's immune system, because infusion of FO into rats also receiving low-dose endotoxin decreased the number of viable bacteria in mesenteric lymph nodes and liver (157). FO did not decrease bacterial translocation across the gut and so the authors concluded that it must have improved bacterial killing.
Studies with parenteral FO in surgical patients
Intravenous infusion of FO into patients for 5 d after gastrointestinal surgery has been shown to alter the FA composition of leukocytes in that the EPA content was increased 2.5-fold (152). This would be expected to affect the profile of eicosanoids produced from AA and EPA. Indeed, several studies have shown that the infusion of FO into such postoperative patients lowers the production of AA-derived leukotrienes (eg, leukotriene B4 and leukotriene C4) and thromboxanes (eg, thromboxane A2) and increases the production of EPA-derived leukotrienes (eg, leukotriene B5, leukotriene B5 isomers, and leukotriene C5) by blood leukocytes stimulated ex vivo (158-161).
Several studies have focused on clinical outcomes in response to the influence of parenteral FO in surgical patients. Importantly, no deleterious immunologic effects of FO infusion were observed in these patients. Furthermore, the only one of these fairly small studies to have examined hard endpoints, such as length of hospital stay, suggests real clinical benefits of fish-oil infusion in these patients (162). In this study, Omegaven was infused, providing 10 g FO/d, on the day before abdominal surgery and for 5 d after abdominal surgery (162). On days 4 and 5, the patients also received standard TPN, which included 50 g fat/d as SO. No differences in infection rates or mortality were observed. However, the postoperative stay in intensive medical wards was significantly shorter in the fish-oil group as was the total hospital stay. The postoperative stay on medical wards was significantly shorter in the fish-oil group. A more recent report from a larger cohort of patients receiving parenteral nutrition after surgery does indicate a benefit of including FO in the regimen (163). There were no differences between the control group (50%:50% SO-MCT) and the patients receiving FO (a mix of Omegaven with the 50%:50% SO-MCT mix, in which a maximum of one-third of the mix was as FO) with respect to the proportion of patients who developed wound infections or who died or in the length of hospital stay. However the proportion of patients in the fish-oil group who were readmitted to intensive care was significantly lower than in the control group. A group of patients also received the FO-containing emulsion for 2 d after surgery. Here there were a number of very significant benefits. This group had a decreased need for mechanical ventilation, a shorter length of hospital stay, less of a need for readmission to intensive care, and lower mortality (163). Another study showed that intravenous infusion of a lipid emulsion containing SO and FO (80%:20%, by vol) into patients for 5 d after major gastrointestinal surgery accelerated the normalization of liver and pancreatic function compared with soybean oil alone. Overall, there was no difference between the groups with respect to length of stay in the intensive care unit or in the hospital. However, in a subgroup of patients at risk of sepsis, there was a reduced intensive care unit stay in the patients who received FO (164). In a recently published study, a mixed group of >650 patients, including 230 postsurgical patients, received parenteral nutrition including FO at 0.11 g/kg per day for 3 d; there were significantly lower rates of infections, fewer complications, and shorter hospital stays in postsurgical patients who received FO than in those who received the control emulsion (165). These authors identified that infusion of 0.15 g FO/kg per day decreased the mean intensive care unit stay and hospital stay. In postsurgical patients who received SO or a mix of SO and FO (80:20, by vol) for 5 d, sepsis incidence, deaths in the intensive care unit, length of intensive care unit stay, and length of hospital stay all tended to decrease in the patients receiving FO, although none of these differences was significant (160). Another group reported a significantly lower length of hospital stay in patients who received a mix of MCT, SO, and FO (50:40:10; Lipoplus) after gastrointestinal surgery than in patients who received SO alone (166). Although some of these studies have been published only in abstract form and further details are required for them to be evaluated more fully, the findings from published studies in gastrointestinal surgical patients clearly show a clinical benefit of the inclusion of long-chain nC3 PUFAs in parenteral nutrition regimens (162-165). However, the study by Tsekos et al (163) also showed a much greater benefit when FAs were additionally provided before surgery, which, of course, is only possible in elective surgery The greater benefit of preoperative infusion of long-chain nC3 PUFAs may relate to better incorporation of the FAs into leukocytes and other tissues.
As previously mentioned, FO-induced modulation of the production of inflammatory mediators appears to play a crucial role in its beneficial clinical effects. Plasma TNF- concentrations were lower (day 6), whereas plasma IL-6 concentrations were lower (day 10) after surgery in patients who had undergone major gastrointestinal surgery and then received a mix of SO, MCT, and FO (30%:50%:20% by vol) for 5 days after surgery compared with those who received SO-MCT (50%:50% by vol) (159). In a more recent study, Omegaven was infused on the day before abdominal surgery and for 5 d after abdominal surgery (162). On days 4 and 5, the patients also received standard TPN, which included 50 g fat/d as SO. TNF- production by endotoxin-stimulated whole blood tended to be lower (day 5) in the fish-oil group, but not significantly so. Postoperative serum IL-6 concentrations were significantly lower in the fish-oil group than in the control group. Monocyte expression of human leukocyte class II antigens of the DR type was preserved in the fish-oil group, but declined after surgery in the control group. Another study compared the effects of lipid-free TPN or lipid-based TPN including SO or a mix of 83% SO and 17% FO (Omegaven) for 5 d after large-bowel surgery (167). There were no differences between the groups with respect to the numbers of circulating lymphocyte populations before or after surgery. Also, there were no differences between groups with respect to T lymphocyte proliferation, but IL-2 production increased in the fish-oil group, and FO prevented the postsurgery decline in interferon production. Taken together, these studies indicate that inclusion of FO in TPN regimens for gastrointestinal surgical patients modulates the generation of inflammatory eicosanoids and cytokines and may help to counter the surgery-induced decline in antigen presenting cell activity and T lymphocyte cytokine production (158, 159, 161, 162, 167).
Studies with parenteral FO in patients with sepsis
It has been shown that fish-oil infusion in patients with sepsis might be associated with clinical improvements. Grecu et al (168) reported significantly lower reoperation rates, intensive care unit stays, and hospital stays in patients who received parenteral FO (as a 66% SO and 33% FO mix) than in those who received SO, but there was no difference in mortality between the 2 groups. Heller et al (165) included 268 patients with abdominal sepsis in their study of parenteral nC3 PUFA infusion. They found a significantly lower rate of infection and shorter lengths of intensive care unit and hospital stay in those patients receiving >0.05 g FO/kg per day than in those receiving less than this. Mortality was significantly decreased in those patients who received >1 g FO/kg per day. Thus, these recent data are also strongly suggestive of genuine clinical benefit from the inclusion of long-chain nC3 PUFAs in parenteral nutrition regimens given to patients with sepsis.
Several studies establish that infusion of long-chain nC3 PUFAs into patients with sepsis can modulate inflammatory mediator production and related inflammatory processes. Infusion of a mix of SO and FO (66%:33%, by vol) over 5 d significantly decreased serum C-reactive protein (CRP) concentrations by an average of 88% in patients with abdominal sepsis; parenteral SO alone did not significantly alter the CRP concentration (168). Septic patients who were intolerant of enteral nutrition received an SO-based emulsion or an emulsion containing FO for 5 or 10 d (169, 170). Blood leukocyte counts and serum CRP concentrations tended to be lower and the production of leukotriene B5 by stimulated neutrophils was significantly higher in patients who received FO (169). Production of TNF-, IL-1, IL-6, IL-8, and IL-10 by endotoxin-stimulated mononuclear cells did not increase during infusion of FO, whereas the production of the 4 proinflammatory cytokines was markedly elevated during the first 2 d of SO infusion (170).
Complex mixed-type emulsions including SO, MCT, OO, and FO
It has been argued that the ratio of nC6 to nC3 PUFAs in parenteral lipids, to support the immune system, should mirror the nutritional environment in which human evolution took place (8, 171). This view is bolstered by observations in an animal transplant model in which the infusion of an emulsion with a ratio of nC6 to nC3 PUFAs of 2:1 showed immune-neutral characteristics, in the form of a maximally reduced graft organ survival, whereas graft survival gradually increased with both lower or higher ratios of nC6 to nC3 PUFAs (171, 172). In line with these findings, a novel emulsion has been developed. This so-called SMOFlipid (Fresenius-Kabi) is a 20% lipid emulsion with the lipid being a mix of 30% MCT, 30% SO, 25% OO, and 15% FO, resulting in a ratio of nC6 to nC3 PUFAs of 2.5:1. A recent phase I study reported that a short infusion (6 h) of SMOF at a rate of 0.125 g fat/kg body weight per hour in healthy male volunteers, when compared with pure SO (Lipovenoes; Fresenius-Kabi), was well tolerated and increased plasma elimination, as evidenced by a less marked increase in serum triacylglycerol concentration and, at the end of infusion, lower serum triacylglycerol concentrations (173). Effects of SMOF and SO on liver function and oxidative stress have been compared in metabolically stressed patients, with SMOF showing slightly dampened liver enzyme abnormalities and increased plasma concentrations of antioxidants (174). A double-blind, randomized study compared TPN based on SMOF or on SO in patients for 5 d after major abdominal surgery (175). Again, SMOF, administered at a dose of 1.5 g fat/kg body weight per day, was well tolerated and increased plasma nC3 FA concentrations and decreased nC6 FA concentrations. SMOF also increased plasma EPA and DHA concentrations but had no effect on AA. Neutrophil leukotriene B5 release was enhanced on day 6 with SMOF, and the length of hospital stay decreased by 7 d (13 compared with 20 d). These data corroborate findings in an earlier study, in which the length of hospital stay in postgastrointestinal surgery patients decreased more with SMOF than with SO (13 compared with 20 d) (176). A recent trial randomly assigned 200 patients after elective abdominal or thoracic surgery to receive TPN based on either SMOF or SO for 5 d postoperatively (177). Although both emulsions were well tolerated and relevant laboratory variables were not different between groups, a trend toward a reduced length of hospital stay was observed with SMOF (16 compared with 18 d). The specific immunologic characteristics of SMOF remain to be characterized.
CONCLUSION
Patients with severe intestinal failure can be successfully treated with TPN for long periods. The foremost threats to patient survival are the underlying condition leading to gut malfunction and infectious complications. Lipids are an established component of TPN, and the lipid component of TPN solutions has traditionally been in the form of SO. There is a view that SO represents an imbalanced FA supply, with an overabundance of nC6 PUFAs. Hard evidence that SO-based lipid emulsions have adverse immunologic effects is lacking. Nevertheless, alternatives to using pure SO have been developed and are in use in some countries. Emulsions that include MCT, OO, and FO as a partial replacement for SO are available. Evidence to date is that these emulsions all offer some advantages over the use of SO alone, although there is a lack of sufficient data on the immunologic consequences and on clinical endpoints. However, promising results in recent studies, especially in those that used FO-based lipids, are encouraging. Clearly, more work to evaluate these emulsions in various clinical settings and to understand the mechanisms of action for their effects are needed.
ACKNOWLEDGMENTS
The author's responsibilities were as follows?GJAW: provided the idea for the study; GJAW and PCC: reviewed the manuscript. The authors had no conflicts of interest to report.
【】
Messing B, Joly F. Guidelines for management of home parenteral support in adult chronic intestinal failure patients. Gastroenterology 2006;130:S43C53.
August D, Teitelbaum D, Albina J, et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr 2002;26:1C138SA.
Grant J. Recognition, prevention, and treatment of home total parenteral nutrition central venous access complications. JPEN J Parenter Enteral Nutr 2002;26(suppl):S21C8.
Koretz RL, Lipman TO, Klein S, American Gastroenterological Association. AGA technical review on parenteral nutrition. Gastroenterology 2001;121:970C1001.
Howard L, Ashley C. Management of complications in patients receiving home parenteral nutrition. Gastroenterology 2003;124:1651C61.
Forbes A. Achieving and maintaining venous access for home parenteral nutrition. Curr Opin Clin Nutr Metab Care 2005;8:285C9.
Heyland DK, MacDonald S, Keefe L, Drover JW. Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA 1998;280:2013C9.
Grimble R. Fatty acid profile of modern lipid emulsions: scientific considerations for creating the ideal composition. Clin Nutr 2005;24(supp):S1C9.
Vinnars E, Hammerqvist L. 25th Arvid Wretlind's lecture. Silver anniversary, 25 years with ESPEN, the history of nutrition. Clin Nutr 2004;23:955C62.
Studley HO. Percentage weight loss. A basic indicator of surgical risk in patients with chronic peptic ulcer. JAMA 1936;106:458C66.
Schuberth O, Wretlind A. Intravenous infusion of fat emulsions, phosphatides and emulsifying agents. Acta Chir Scand 1961;13(suppl):S278C84.
Edgren B, Wretlind A. The theoretical background of the intravenous nutrition with fat emulsions. Nutr Dieta Eur Rev Nutr Diet 1963;13:364C86.
Hallberg D, Schuberth O, Wretlind A. Experimental and clinical studies with fat emulsion for intravenous nutrition. Nutr Dieta Eur Rev Nutr Diet 1966;8:245C81.
Wretlind A. Complete intravenous nutrition. Theoretical and experimental background. Nutr Metab 1972;14(suppl):1C57.
Dudrick SJ, Wilmore DW, Hars HM, et al. Long-term total parenteral nutrition with growth, development, and positive nitrogen balance. Surgery 1968;64:134C42.
Dudrick SJ. Early developments and clinical applications of total parenteral nutrition. JPEN J Parenter Enteral Nutr 2003;27:291C9.
Wretlind A. Development of fat emulsions. JPEN J Parenter Enteral Nutr 1981;5:230C5.
Carpentier Y. Substrates used in parenteral and enteral nutrition: lipids. In: Sobotka L, ed. Basics in clinical nutrition. 3rd ed. Prague, Czech Republic: Publishing House Galen, 2004:153C6.
Klein S, Miles JM. Metabolic effects of long-chain and medium-chain triacylglycerols in humans. JPEN J Parenter Eneteral Nutr 1994;18:396C7.
Abbott WC, Grakauskas AM, Bistrian BR, Rose R, Blackburn GL. Metabolic and respiratory effects of continuous and discontinuous lipid infusions. Occurrence in excess of resting energy expenditure. Arch Surg 1984;119:1367C71.
Jensen GL, Mascioli EA, Seidner DL, et al. Parenteral infusion of long- and medium-chain triglycerides and reticuloendothelial system function in man. JPEN J Parenter Enteral Nutr 1990;14:467C71.
Driscoll DF, Adolph M, Bistrian M. Lipid emulsions in parenteral nutrition. In: Rombeau JL, Rolandelli RH, eds. Clinical nutrition: parenteral nutrition. 3rd ed. Philadelphia, PA: WB Saunders, 2001:35C9.
Carpentier YA, Simoens C, Siderova V, et al. Recent developments in lipid emulsions: relevance to intensive care. Nutrition 1997;13(suppl):S73C8.
Ferezou J, Bach A. Structure and metabolic fate of triacylglycerol- and phospholipid-rich particles of commercial parenteral fat emulsions. Nutrition 1999;15:44C50.
Iriyama K, Nishiwaki H, Terashima H, et al. Apolipoprotein C-II modifications associated with an infusion of artificial lipid particles. JPEN J Parenter Enteral Nutr 1988;12:60C2.
Melin T, Qi C, Bengtsson-Olivecrona G, Akesson B, Nilsson A. Hydrolysis of chylomicron polyenoic fatty acid esters with lipoprotein lipase and hepatic lipase. Biochim Biophys Acta 1991;1075:259C66.
Kalfarentzos F, Kokkinis K, Leukaditi K, Maroulis J, Onoufriou A, Alexopoulos K. Comparison between two fat emulsions: Intralipid 30 cent vs intralipid 10 cent in critically ill patients. Clin Nutr 1998;17:31C4.
Wanten G, Beunk J, Naber T, Swinkels D. Tocopherol isoforms in parenteral lipid emulsions and neutrophil activation. Clin Nutr 2002;21:417C22.
Steger PJ, Muhlebach SF. Lipid peroxidation of i.v. lipid emulsions in TPN bags: the influence of tocopherols. Nutrition 1998;14:179C85.
Steger PJ, Muhlebach SF. Lipid peroxidation of intravenous lipid emulsions and all-in-one admixtures in total parenteral nutrition bags: the influence of trace elements. JPEN J Parenter Enteral Nutr 2000;24:37C41.
Gunstone FD. High resolution 13C NMR. A technique for the study of lipid structure and composition. Prog Lipid Res 1994;33:19C28.
Calder PC. Polyunsaturated fatty acids, inflammation and immunity. Lipids 2001;36:1007C24.
Wanten G, Janssen F, Naber A. Saturated triglycerides and fatty acids activate neutrophils depending on carbon chain-length. Eur J Clin Invest 2002;32:285C9.
Calder PC. Dietary modification of inflammation with lipids. Proc Nutr Soc 2002;61:345C58.
Yaqoob P. fatty acids as gatekeepers of immune cell regulatioin. Trends Immunol 2003;24:639C45.
Yaqoob P. Fatty acids and the immune system: from basic science to clinical applications. Proc Nutr Soc 2004;63:89C104.
Calder PC, Yaqoob P, Harvey DJ, Watts A, Newsholme EA. Incorporation of fatty acids by concanavalin A-stimulated lymphocytes and the effect on fatty acid composition and membrane fluidity. Biochem J 1994;300:509C18.
Wanten G, Naber A. Human neutrophil membrane fluidity after exposure to structurally different lipid emulsions. JPEN J Parenter Enteral Nutr 2001;25:352C5.
Marmor MD, Julius M. Role for lipid rafts in regulating interleukin-2 receptor signaling. Blood 2001;98:1489C97.
Larbi A, Grenier A, Frisch F, et al. Acute in vivo elevation of intravascular triacylglycerol lipolysis impairs peripheral T cell activation in humans. Am J Clin Nutr 2005;82:949C56.
Stulnig TM, Huber J, Leitinger N, et al. Polyunsaturated eicosapentaenoic acid displaces proteins from membrane rafts by altering raft lipid composition. J Biol Chem 2001;276:37335C40.
Lewis RA. Interactions of eicosanoids and cytokines in immune regulation. Adv Prostaglandin Thromboxane Leukot Res 1990;20:170C8.
Tilley SL, Coffman TM, Koller BH. Mixed messages: modulation of inflammation and immune responses by prostaglandins and thromboxanes. J Clin Invest 2001;108:15C23.
Serhan CN, Arita M, Hong S, Gotlinger K. Resolvins, docosatrienes, and neuroprotectins, novel omega-3-derived mediators, and their endogenous aspirin-triggered epimers. Lipids 2004;39:1125C32.
Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nat Immunol 2005;6:1191C7.
Arita M, Clish CB, Serhan CN. The contributions of aspirin and microbial oxygenase to the biosynthesis of anti-inflammatory resolvins: novel oxygenase products from omega-3 polyunsaturated fatty acids. Biochem Biophys Res Commun 2005;338:149C57.
Serhan CN, Haeggstrom JZ, Leslie CC. Lipid mediator networks in cell signaling: update and impact of cytokines. FASEB J 1996;10:1147C58.
Yaqoob P. Lipids and the immune response. Curr Opin Clin Nutr Metab Care 1998;1:153C61.
Wanten G, van Emst-de Vries S, Naber T, Willems P. Nutritional lipid emulsions modulate cellular signaling and activation of human neutrophils. J Lipid Res 2001;42:428C36.
Wanten G, Rops A, van Emst-de Vries S, Naber T, Willems P. Prompt inhibition of fMLP-induced Ca2+ mobilization by parenteral lipid emulsions in human neutrophils. J Lipid Res 2002;43:550C6.
Underhill DM, Ozinsky A. Toll-like receptors: key mediators of micobe detection. Curr Opin Immunol 2002;14:103C10.
Lee JY, Sohn KH, Rhee SH, Hwang D. Saturated fatty acids, but not unsaturated fatty acids induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem 2001;276:16683C9.
Lee JY, Plakidas A, Lee WH, et al. Differential modulation of Toll-like receptors by fatty acids: preferential inhibition by nC3 polyunsaturated fatty acids. J Lipid Res 2003;44:479C86.
Netea MG, van der Meer JW, Sutmuller RP, Adema GJ, Kullberg BJ. From the Th1/Th2 paradigm towards a Toll-like receptor/T-helper bias. Antimicrob Agents Chemother 2005;10:3991C6.
Deckelbaum RJ, Worgall TS, Seo T. nC3 Fatty acids and gene expression. Am J Clin Nutr 2006;83(suppl):S1520C5.
Cury-Boaventura MF, Gorjao R, de Lima TM, Newsholme P, Curi R. Comparative toxicity of oleic and linoleic acid on human lymphocytes. Life Sci 2006;78:1448C56.
Switzer KC, McMurray DN, Morris JS, Chapkin RS. nC3 Polyunsaturated fatty acids promote activation-induced cell death in murine T lymphocytes. J Nutr 2003;133:496C503.
Bansal V, Syres KM, Makarenkova V, et al. Interactions between fatty acids and arginine metabolism: implications for the design of immune-enhancing diets. JPEN J Parenter Enteral Nutr 2005;29(suppl):S75C80.
Furukawa K, Yamamori H, Takagi K, et al. Influences of soybean oil emulsion on stress response and cell-mediated immune function in moderately or severely stressed patients. Nutrition 2002;18:235C40.
Heyland DK. Parenteral nutrition in critically ill patients: more harm than good. Proc Nutr Soc 2000;59:457C66.
Jarvis WR, Highsmith AK, Allen JR, Haley RW. Polymicrobial bacteremia associated with lipid emulsion in a neonatal intensive care unit. Pediatr Infect Dis 1983;2:203C8.
Freeman J, Goldmann DA, Smith NE, Sidebottom DG, Epstein MF, Platt R. Association of intravenous lipid emulsions and coagulase-negative staphylococcal bacteremia in neonatal intensive care units. N Engl J Med 1990;323:301C8.
Goldmann DA. Coagulase-negative staphylococci: interplay of epidemiology and bench research. Am J Infect Control 1990;18:211C21.
Snydman DR, Murray SA, Kornfeld SJ, Majka JA, Ellis CA. Total parenteral nutrition-related infections Am J Med 1982;73:695C71.
The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. Perioperative total parenteral nutrition in surgical patients. N Engl J Med 1991;325:525C32.
Muscaritoli M, Conversano L, Torelli GF, et al. Clinical and metabolic effects of different parenteral nutrition regimens in patients undergoing allogeneic bone marrow transplantation. Transplantation 1998;66:610C6.
Lenssen P, Bruemmer BA, Bowden RA, Gooley T, Aker SA, Mattson D. Intravenous lipid dose and incidence of bacteremia and fungemia in patients undergoing bone marrow transplantation. Am J Clin Nutr 1998;67:927C33.
Wiernik A, Jarstrand C, Julander I. The effect of intralipid on mononuclear and polymorphonuclear phagocytes. Am J Clin Nutr 1983;37:256C61.
Nordenstrom J, Jarstrand C, Wiernik A. Decreased chemotactic and random migration of leukocytes during Intralipid infusion. Am J Clin Nutr 1979;32:2416C22.
English D, Roloff JS, Lukens JN, Parker P, Greene HL, Ghishan FK. Intravenous lipid emulsions and human neutrophil function. J Pediatr 1981;99:913C6.
Fischer GW, Hunter KW, Wilson SR, Mease AD. Diminished bacterial defences with intralipid. Lancet 1980;2:819C20.
Palmblad J. Intravenous lipid emulsions and host defense: a critical review. Clin Nutr 1991;10:303C8.
Seidner DL, Mascioli EA, Istfan NW, et al. Effects of long-chain triglyceride emulsions on reticuloendothelial system function in humans. JPEN J Parenter Enteral Nutr 1989;13:614C9.
Jarstrand C, Rasool O. Intralipid decreases the bacterial lipopolysaccharide induced release of oxygen radicals and lysozyme from human neutrophils. Scand J Infect Dis 1991;23:481C7.
Duran B. The effects of long-term total parenteral nutrition on gut mucosal immunity in children with short bowel syndrome: a systematic review. BMC Nurs 2005;4:2C12.
Waitzberg DL, Lotierzo PH, Logullo AF, Torrinhas RS, Pereira CC, Meier R. Parenteral lipid emulsions and phagocytic systems. Br J Nutr 2002;87(suppl):S49C57.
Wanten GJ, Naber AH, Netea M. Modulation of inflammatory cytokine production by parenteral lipid emulsions. Clin Nutr 2005;24:164C5.
Bellinati-Pires R, Waitzberg DL, Salgado MM, Carneiro-Sampaio MM. Effect of medium- and long-chain triglycerides on human neutrophil migration. Braz J Med Biol Res 1992;25:369C73.
Palmblad J, Brostrom O, Lahnborg G, Uden AM, Venizelos N. Neutrophil functions during total parenteral nutrition and Intralipid infusion. Am J Clin Nutr 1982;35:1430C6.
Robin AP, Arain I, Phuangsab A, Holian O, Roccaforte P, Barrett JA. Intravenous fat emulsion acutely suppresses neutrophil chemiluminescence. JPEN J Parenter Enteral Nutr 1989;13:608C13.
Usmani SS, Harper RG, Usmani SF. Effect of a lipid emulsion (Intralipid) on polymorphonuclear leukocyte functions in the neonate. J Pediatr 1988;113:132C6.
Rasmussen A, Hessov I, Segel E. The effect of Intralipid on polymorphonuclear leukocytes. Clin Nutr 1988;7:37C41.
Escudier EF, Escudier BJ, Henry Amar MC, et al. Effects of infused intralipids on neutrophil chemotaxis during total parenteral nutrition. JPEN J Parenter Enteral Nutr 1986;10:596C98.
Bach AC, Storck D, Meraihi, Z. Medium-chain triglyceride-based fat emulsions: an alternative energy supply in stress and sepsis. JPEN J Parenter Enteral Nutr 1988;12:S82C8.
Bach AC, Babayan VK. Medium-chain triglycerides: an update. Am J Clin Nutr 1982;36:950C62.
Groot PH, Hulsmann WC. The activation and oxidation of octanoate and palmitate by rat skeletal muscle mitochondria. Biochim Biophys Acta 1973;316:124C35.
Patet G, Thelin A, Philipposian G, et al. In: Horisberger M, Bracco U, eds. Lipids in modern nutrition. New York, NY: Raven Press, 1987:43C7.
Deckelbaum RJ, Hamilton JA, Moser A, et al. Medium-chain versus long-chain triacylglycerol emulsion hydrolysis by lipoprotein lipase and hepatic lipase: implications for the mechanisms of lipase action. Biochemistry 1990;29:1136C42.
Oliveira FL, Rumsey SC, Schlotzer E, Hansen I, Carpentier YA, Deckelbaum RJ. Triglyceride hydrolysis of soy oil vs fish oil emulsions. JPEN J Parenter Enteral Nutr 1997;21:224C9.
Ulrich H, Pastores SM, Katz DP, Kvetan V. Parenteral use of medium-chain triglycerides: a reappraisal. Nutrition 1996;12:231C8.
Kuse ER, Kotzerke J, Muller S, Nashan B, Luck R, Jaeger K. Hepatic reticuloendothelial function during parenteral nutrition including an MCT/LCT or LCT emulsion after liver transplantation?a double-blind study. Transpl Int 2002;15:272C7.
Stouthard JM, Endert E, Romijn JA, Sauerwein HP. Infusion of long-chain or medium-chain triglycerides inhibits peripheral glucose metabolism in men. JPEN J Parenter Enter Nutr 1994;18:436C41.
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359C67.
Sidossis LS, Stuart CA, Shulman GI, Lopaschuk GD, Wolfe RR. Glucose plus insulin regulate fat oxidation by controlling the rate of fatty acid entry into the mitochondria. J Clin Invest 1996;98:2244C50.
Chan S, McCowen KC, Bistrian B. Medium-chain triglyceride and nC3 polyunsaturated fatty acid-containing emulsions in intravenous nutrition. Curr Opin Clin Nutr Metab Care 1998;1:163C9.
Ball MJ, White K. Comparison of medium and long chain triglyceride metabolism in intensive care patients on parenteral nutrition. Intensive Care Med 1989;15:250C4.
Ball MJ, White K. Metabolic effects of intravenous medium- and long-chain triacylglycerols in critically ill patients. Clin Sci 1989;76:165C70.
Ball MJ. Parenteral nutrition in the critically ill: use of a medium chain triglyceride emulsion. Intensive Care Med 1993;19:89C95.
Garnacho-Montero J, Ortiz-Leyba C, Jimenez-Jimenez FJ, et al. Clinical and metabolic effects of two lipid emulsions on the parenteral nutrition of septic patients. Nutrition 2002;18:134C8.
Grau T, Ruiz de Adana JC, Zubillega S, Fuerte S, Giron C. Randomized study of two different fat emulsions in total parenteral nutrition of malnourished surgical patients; effect of infectious morbidity and mortality. Nutr Hosp 2003;18:159C66.
Lekka ME, Liokatis S, Nathanail C, Galani V, Nakos G. The impact of intravenous fat emulsion administration in acute lung injury. Am J Respir Crit Care Med 2004;169:638C44.
Smirniotis V, Kostopanagiotou G, Vassiliou J, et al. Long chain versus medium chain lipids in patients with ARDS: effects on pulmonary haemodynamics and gas exchange. Intensive Care Med 1998;24:1029C33.
Wanten GJ, Naber AH. Cellular and physiological effects of medium-chain triglycerides. Mini Rev Med Chem 2004;4:847C57.
Wanten GJ, Geijtenbeek TB, Raymakers RA, et al. Medium-chain, triglyceride-containing lipid emulsions increase human neutrophil beta2 integrin expression, adhesion, and degranulation. JPEN J Parenter Enteral Nutr 2000;24:228C33.
Versleijen M, Roelofs H, Preijers F, Roos D, Wanten G. Parenteral lipids modulate leukocyte phenotypes in whole blood, depending on their fatty acid composition. Clin Nutr 2005;24:822C9.
Wanten GJ, Roos D, Naber AH. Effects of structurally different lipid emulsions on human neutrophil migration. Clin Nutr 2000;19:327C31.
Wanten GJ, Curfs JH, Meis JF, Naber AH. Phagocytosis and killing of Candida albicans by human neutrophils after exposure to structurally different lipid emulsions. JPEN J Parenter Enteral Nutr 2001;25:9C13.
Han JR, Farmer SR, Kirkland JL, et al. Octanoate attenuates adipogenesis in 3T3CL1 preadipocytes. J Nutr 2002;132:904C10.
Wanten G. An update on parenteral lipids and immune function: only smoke, or is there any fire? Curr Opin Clin Nutr Metab Care 2006;9:79C83.
Sandstrom R, Hyltander A, Korner U, Lundholm K. Structured triglycerides were well tolerated and induced increased whole body fat oxidation compared with long-chain triglycerides in postoperative patients. JPEN J Parenter Enteral Nutr 1995;19:381C6.
Sandstrom R, Hyltander A, Korner U, Lundholm K. Structured triglycerides to postoperative patients: a safety and tolerance study. JPEN J Parenter Enteral Nutr 1993;17:153C7.
Hedeman H, Brondsted H, Mullertz A, Frokjaer S. Fat emulsions based on structured lipids (1,3-specific triglycerides): an investigation of the in vivo fate. Pharm Res 1996;13:725C8.
Kruimel JW, Naber TH, Van der Vliet JA, Carneheim C, Katan MB, Jansen JB. Parenteral structured triglyceride emulsion improves nitrogen balance and is cleared faster from the blood in moderately catabolic patients. JPEN J Parenter Enteral Nutr 2001;25:237C44.
Waitzberg DL, Torrinhas RS, Jacintho TM. New parenteral lipid emulsions for clinical use. JPEN J Parenter Enteral Nutr 2006;30:351C67.
Chambrier C, Lauverjat M, Bouletreau P. Structured triglyceride emulsions in parenteral nutrition. Nutr Clin Pract 2006;21:342C50.
Nakagawa M, Hiramatsu Y, Mitsuyoshi K, Yamamura M, Hioki K, Yamamoto M. Effect of various lipid emulsions on total parenteral nutrition-induced hepatosteatosis in rats. JPEN J Parenter Enteral Nutr 1991;15:137C43.
Reimund JM, Rahmi G, Escalin G, et al. Efficacy and safety of an olive oil-based intravenous fat emulsion in adult patients on home parenteral nutrition. Aliment Pharmacol Ther 2005;21:445C54.
Goulet O, de Potter S, Antebi H, et al. Long-term efficacy and safety of a new olive oil-based intravenous fat emulsion in pediatric patients: a double-blind randomized study. Am J Clin Nutr 1999;70:338C45.
Thomas-Gibson S, Jawhari A, Atlan P, Brun AL, Farthing M, Forbes A. Safe and efficacious prolonged use of an olive oil-based lipid emulsion (ClinOleic) in chronic intestinal failure. Clin Nutr 2004;23:697C703.
Reimund JM, Arondel Y, Joly F, Messing B, Duclos B, Baumann R. Potential usefulness of olive oil-based lipid emulsions in selected situations of home parenteral nutrition-associated liver disease. Clin Nutr 2004;23:1418C25.
Huschak G, Zur Nieden K, Hoell T, Riemann D, Mast H, Stuttmann R. Olive oil based nutrition in multiple trauma patients: a pilot study. Intensive Care Med 2005;31:1202C8.
Yaqoob P, Knapper JA, Webb DH, Williams CM, Newsholme EA, Calder PC. Effect of olive oil on immune function in middle-aged men. Am J Clin Nutr 1998;67:129C35.
Granato D, Blum S, Rossle C, Le Boucher J, Malnoe A, Dutot G. Effects of parenteral lipid emulsions with different fatty acid composition on immune cell functions in vitro. JPEN J Parenter Enteral Nutr 2000;24:113C8.
Reimund JM, Scheer O, Muller CD, Pinna G, Duclos B, Baumann R. In vitro modulation of inflammatory cytokine production by three lipid emulsions with different fatty acid compositions. Clin Nutr 2004;23:1324C32.
Buenestado A, Cortijo J, Sanz MJ, et al. Olive oil-based lipid emulsion's neutral effects on neutrophil functions and leukocyte-endothelial cell interactions. JPEN J Parenter Enteral Nutr 2006;30:286C96.
Moussa M, Le Boucher J, Garcia J, et al. In vivo effects of olive oil-based lipid emulsion on lymphocyte activation in rats. Clin Nutr 2000;19:49C54.
Garnacho-Montero J, Ortiz-Leyba C, Garnacho-Montero MC, et al. Effects of three intravenous lipid emulsions on the survival and mononuclear phagocyte function of septic rats. Nutrition 2002;18:751C4.
Schepens MA, Roelofs HM, Peters WH, Wanten GJ. No evidence for oxidative stress in patients on home parenteral nutrition. Clin Nutr 2006;25:939C48
Qi K, Al-Haideri M, Seo T, Carpentier YA, Deckelbaum RJ. Effects of particle size on blood clearance and tissue uptake of lipid emulsions with different triglyceride compositions. JPEN J Parenter Enteral Nutr 2003;27:58C64.
Ton M, Chang C, Carpentier Y, Deckelbaum RJ. In vivo and in vitro properties of an intravenous lipid emulsion containing only medium chain and fish oil triglycerides. Clin Nutr 2005;24:492C501.
Mascioli EA, Iwasa Y, Trimbo S, Leader L, Bistrian BR, Blackburn GL. Endotoxin challenge after menhaden oil diet: effects on survival of guinea pigs. Am J Clin Nutr 1989;49:277C82.
Mascioli E, Leader L, Flores E, Trimbo S, Bistrian B, Blackburn G. Enhanced survival to endotoxin in guinea pigs fed IV fish oil emulsion. Lipids 1988;23:623C5.
Utsunomiya T, Chavali SR, Zhong WW, Forse RA. Effects of continuous tube feeding of dietary fat emulsions on eicosanoid production and on fatty acid composition during an acute septic shock in rats. Biochim Biophys Acta 1994;1214:333C9.
Sane S, Baba M, Kusano C, et al. Eicosapentaenoic acid reduces pulmonary edema in endotoxemic rats. J Surg Res 2000;93:21C7.
Sadeghi S, Wallace FA, Calder PC. Dietary lipids modify the cytokine response to bacterial lipopolysaccharide in mice. Immunology 1999;96:404C10.
Pomposelli JJ, Flores EA, Blackburn GL, Zeisel SH, Bistrian BR. Diets enriched with nC3 fatty acids ameliorate lactic acidosis by improving endotoxin-induced tissue hypoperfusion in guinea pigs. Ann Surg 1991;213:166C76.
Teo TC, Selleck KM, Wan JM, et al. Long-term feeding with structured lipid composed of medium-chain and nC3 fatty acids ameliorates endotoxic shock in guinea pigs. Metabolism 1991;40:1152C9.
Murray MJ, Kanazi G, Moukabary K, Tazelaar HD, DeMichele SJ. Effects of eicosapentaenoic and gamma-linolenic acids (dietary lipids) on pulmonary surfactant composition and function during porcine endotoxemia. Chest 2000;117:1720C7.
Mancuso P, Whelan J, DeMichele SJ, Snider CC, Guszcza JA, Karlstad MD. Dietary fish oil and fish and borage oil suppress intrapulmonary proinflammatory eicosanoid biosynthesis and attenuate pulmonary neutrophil accumulation in endotoxic rats. Crit Care Med 1997;25:1198C206.
Mancuso P, Whelan J, DeMichele SJ, et al. Effects of eicosapentaenoic and gamma-linolenic acid on lung permeability and alveolar macrophage eicosanoid synthesis in endotoxic rats. Crit Care Med 1997;25:523C32.
Murray MJ, Kumar M, Gregory TJ, Banks PL, Tazelaar HD, DeMichele SJ. Select dietary fatty acids attenuate cardiopulmonary dysfunction during acute lung injury in pigs. Am J Physiol 1995;269:2090C9.
Murray MJ, Svingen BA, Yaksh TL, Holman RT. Effects of endotoxin on pigs prefed omega-3 vs. omega-6 fatty acid-enriched diets. Am J Physiol 1993;265:920C7.
Murray MJ, Svingen BA, Holman RT, Yaksh TL. Effects of a fish oil diet on pigs' cardiopulmonary response to bacteremia. JPEN J Parenter Enteral Nutr 1991;15:152C8.
Barton RG, Wells CL, Carlson A, Singh R, Sullivan JJ, Cerra FB. Dietary omega-3 fatty acids decrease mortality and Kupffer cell prostaglandin E2 production in a rat model of chronic sepsis. J Trauma 1991;31:768C73.
Rayon JI, Carver JD, Wyble LE, et al. The fatty acid composition of maternal diet affects lung prostaglandin E2 levels and survival from group B streptococcal sepsis in neonatal rat pups. J Nutr 1997;127:1989C92.
Lanza-Jacoby S, Flynn JT, Miller S. Parenteral supplementation with a fish-oil emulsion prolongs survival and improves rat lymphocyte function during sepsis. Nutrition 2001;17:112C6.
Johnson JA 3rd, Griswold JA, Muakkassa FF. Essential fatty acids influence survival in sepsis. J Trauma 1993;35:128C31.
Billiar TR, Bankey PE, Svingen BA, et al. Fatty acid intake and Kupffer cell function: fish oil alters eicosanoid and monokine production to endotoxin stimulation. Surgery 1988;104:343C9.
Renier G, Skamene E, DeSanctis J, Radzioch D. Dietary nC3 polyunsaturated fatty acids prevent the development of atherosclerotic lesions in mice. Modulation of macrophage secretory activities. Arterioscler Thromb 1993;13:1515C24.
Yaqoob P, Calder P. Effects of dietary lipid manipulation upon inflammatory mediator production by murine macrophages. Cell Immunol 1995;163:120C8.
Endres S, Ghorbani R, Kelley VE, et al. The effect of dietary supplementation with nC3 polyunsaturated fatty acids on the synthesis of interleukin-1 and tumor necrosis factor by mononuclear cells. N Engl J Med 1989;320:265C71.
Meydani SN, Endres S, Woods MM, et al. Oral (nC3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J Nutr 1991;121:547C55.
Caughey GE, Mantzioris E, Gibson RA, Cleland LG, James MJ. The effect on human tumor necrosis factor alpha and interleukin 1 beta production of diets enriched in nC3 fatty acids from vegetable oil or fish oil. Am J Clin Nutr 1996;63:116C22.
Abbate R, Gori AM, Martini F, et al. nC3 PUFA supplementation, monocyte PCA expression and interleukin-6 production. Prostaglandins Leukot Essent Fatty Acids 1996;54:439C44.
Trebble T, Arden NK, Stroud MA, et al. Inhibition of tumour necrosis factor-alpha and interleukin 6 production by mononuclear cells following dietary fish-oil supplementation in healthy men and response to antioxidant co-supplementation. Br J Nutr 2003;90:405C12.
Wallace FA, Miles EA, Calder PC. Comparison of the effects of linseed oil and different doses of fish oil on mononuclear cell function in healthy human subjects. Br J Nutr 2003;89:679C89.
Pscheidl E, Schywalsky M, Tschaikowsky K, Boke-Prols T. Fish oil-supplemented parenteral diets normalize splanchnic blood flow and improve killing of translocated bacteria in a low-dose endotoxin rat model. Crit Care Med 2000;28:1489C96.
Morlion BJ, Torwesten E, Lessire H, et al. The effect of parenteral fish oil on leukocyte membrane fatty acid composition and leukotriene-synthesizing capacity in patients with postoperative trauma. Metabolism 1996;45:1208C13.
Wachtler P, Konig W, Senkal M, Kemen M, Koller M. Influence of a total parenteral nutrition enriched with omega-3 fatty acids on leukotriene synthesis of peripheral leukocytes and systemic cytokine levels in patients with major surgery. J Trauma 1997;42:191C8.
Kelbel I, Wagner F, Wiedeck-Suger H, et al. Effects of nC3 fatty acids on immune function: a double-blind, randomized trial of fish oil based infusion in post-operative patients. Clin Nutr 2002;21:13C4(abstr).
Koller M, Senkal M, Kemen M, Konig W, Zumtobel V, Muhr G. Impact of omega-3 fatty acid enriched TPN on leukotriene synthesis by leukocytes after major surgery. Clin Nutr 2003;22:59C64.
Weiss G, Meyer F, Matthies B, Pross M, Koenig W, Lippert H. Immunomodulation by perioperative administration of nC3 fatty acids. Br J Nutr 2002;87:89C94.
Tsekos E, Reuter C, Stehle P, Boeden G. Perioperative administration of parenteral fish oil supplements in a routine clinical setting improves patient outcome after major abdominal surgery. Clin Nutr 2004;23:325C30.
Heller AR, Rossel T, Gottschlich B, et al. Omega-3 fatty acids improve liver and pancreas function in postoperative cancer patients. Int J Cancer 2004;111:611C6.
Heller AR, Rossler S, Litz RJ, et al. Omega-3 fatty acids improve the diagnosis-related clinical outcome. Crit Care Med 2006;34:1253C5.
Wichmann MW, Morlion B, Czarnetzki H-D, Thul P, Jauch K-W. Reduction of length of postoperative stay by fish oil containing lipid emulsion?data from a multi-center trial. Clin Nutr 2004;23:1471.
Schauder P, Rohn U, Schafer G, Korff G, Schenk HD. Impact of fish oil enriched total parenteral nutrition on DNA synthesis, cytokine release and receptor expression by lympho-cytes in the postoperative period. Br J Nutr 2002;87:103C10.
Grecu I, Mirea L, Gintescu I. Parenteral fish oil supplementation in patients with abdominal sepsis. Clin Nutr 2003;22:23 (abstr).
Mayer K, Gokorsch S, Fegbeutel C, et al. Parenteral nutrition with fish oil modulates cytokine response in patients with sepsis. Am J Respir Crit Care Med 2003;167:1321C8.
Mayer K, Fegbeutel C, Hattar K, et al. Omega-3 vs. omega-6 lipid emulsions exert differential influence on neutrophils in septic shock patients: impact on plasma fatty acids and lipid mediator generation. Intensive Care Med 2003;29:1472C81.
Grimm H, Tibell A, Norrlind B, Clecher C, Wilker S, Schwemmle K. Immunoregulation by parenteral lipids: impact of the nC3 to nC6 fatty acid ratio. JPEN J Parenter Enteral Nutr 1994;18:417C21.
Grimm H, Tibell A, Norrlind B, Schott J, Bohle RM. Nutrition and allorejection impact of lipids. Transplant Immunol 1995;3:62C7.
Schlotzer E, Kanning U. Elimination and tolerance of a new parenteral lipid emulsion (SMOF)?a double-blind cross-over study in healthy male volunteers. Ann Nutr Metab 2004;48:263C8.
Antebi H, Mansoor O, Ferrier C, et al. Liver function and plasma antioxidant status in intensive care unit patients requiring total parenteral nutrition: comparison of 2 fat emulsions. JPEN J Parenter Enteral Nutr 2004;28:142C8.
Grimm H, Mertes N, Goeters C, et al. Improved fatty acid and leukotriene pattern with a novel lipid emulsion in surgical patients. Eur J Nutr 2006;45:55C60.
Schulzki C, Mertes N, Wenn A, et al. Effects of a new type of lipid emulsion based on soybean oil, MCT, olive oil and fish oil (SMOF) in surgical patients. Clin Nutr 1999;18:7 (abstr).
Mertes N, Grimm H, Furst P, Stehle P. Safety and efficacy of a new parenteral lipid emulsion (SMOFLipid) in surgical patients: a randomized, double-blind, multicenter study. Ann Nutr Metab 2006;50:253C9.