左旋布比卡因用于良性前列腺增生摘除术后患者自控硬膜外镇痛效果及循环应激反应的影响
【关键词】 良性前列腺增生
摘要:目的:研究左旋布比卡因伍用芬太尼在良性前列腺增生摘除术后患者自控硬膜外镇痛效果及循环应激反应的影响。方法:随机选择ASAI-Ⅱ级,年龄55~75岁、择期作良性前列腺增生耻骨上经膀胱前列腺摘除术40例为患者自控硬膜外镇痛组(PCEA组),另随机选择同类手术患者40例为哌替啶肌注镇痛组(PMA组)。在PCEA组镇痛药液为芬太尼0.5mg、氟哌利多5mg和左旋布比卡因187.5mg用生理盐水配至100ml。PMA组当患者疼痛难忍时,每次肌注哌替啶0.8mg/kg。分别采用视觉模拟评分(VAS)评定镇痛效果,监测并记录麻醉前、术毕、术后6、12、24h的BP、HR值,并心率收缩压之积(RPP),同时采肘静脉血,用高效相色谱法测定血浆去甲肾上腺素(NE)和肾上腺素(E)的浓度,术后膀胱冲洗量、出血量膀胱痉挛两组患者例数,镇痛期间的不良反应。结果:术后各时点的VAS评分PCEA组较PMA组显著低(p<0.05或p<0.01)PMA组术后各时点的HR、SBP、RPP、CA及术后6、12h的DBP均较麻醉前明显增高(P<0.05P或<0.01),PCEA组除NE于术后6h较麻醉前高外(P<0.01),其余指标与其麻醉前相比无显著差异(P>0.05),术后各时点的RPP、血浆CA及术后6、12h的SBP、DBP、HR值均明显低于PMA组(P<0.05或P<0.01)。术后膀胱冲洗量、出血量、膀胱痉挛例数PMA组均高于PCEA组(P<0.05)。结论:左旋布比卡因伍用芬太尼在良性前列腺增生摘除术后患者自控硬膜外镇痛效果理想对循环应激反应的影响较小。
关键词: 左旋布比卡因; 硬膜外; 镇 痛; 良性前列腺增生
Effect of PCEA with L-bupivacaine after Benign Prostatectomy and its Influence on Stress Response of Circulation
Abstract: Objective:To study the effect of postoperative patient-controlled epidural analgesia with L- bupivacaine and fentanyl after benign prostatectomy and its influence on the stress response of circulation.Methods:Forty cases ASAⅠ~Ⅱ undergone elective prostatectomy,aged from 55 to 75,were randomly enrolled into the patient-controlled epidural analgesia group(PCEA). Forty other cases suffered the similar symptoms were randomly enrolled into the pethidine intramuscular injection group (PMA).In the PCEA group, 100ml Sodium Chloride contains fentanyl 0.5mg, droperidol 5mg and L-bupivacaine187.5mg. In the PMA group, pethidine 0.8mg/kg was injected each time when the patient can’t bear.The effect was evaluated by visual analogue pain scales.Blood pressure(BP)and heart rate(HR) was monitored and recorded before aneshtesia,at completion of operation and 6 hours, 12 hours, 24 hours postoperatively.The result of HR multiplied by systolic BP was also recorded.At the same time blood sample was taken through ulnar vein.The concentration of plasma NE and E was detected by high performance liquid chromatography .Flushing dose of bladder,hemorrhage volume, the number of patients suffered bladder spasm and adverse reaction postoperatively were recorded in detail.Results:VAS of the PCEA group was significantly lower than that of the PMA group (P<0.05 or P<0.01 ) at each period postoperatively.In the PMA group HR,SBP,RPP,CA at every period and DBP at 6 hours,12 hours postoperatively was significantly higher(P<0.05 or P<0.01) than that of before aneshtesia.Compared with the parameter before aneshtesia , there is no significant different in the PCEA group.Only the NE is significant higher than that of before aneshtesia in the PCEA group.In the PCEA group RPP, plasma CA at every period and SBP,DBP , HR at 6 hours,12 hours postoperatively was significantly lowerer than that of the PMA group (P<0.05 or p<0.01 ). Flushing dose of bladder,hemorrhage volume, the number of patients suffered bladder spasm in the PMA group was significant higher than that of the PCEA group(p<0.05 ).Conclusion: Patient-controlled epidural analgesia with L-bupivacaine and fentanyl postoperatively after benign prostatectomy is highly effective and has little influence on stress response of circulation.
Key words: L-bupivacaine; Epidural; Analgesia; Begin prostate
硬膜外腔持续泵入芬太尼和布比卡因混合液,产生节段性镇痛,效果确切,现已广泛用于术后镇痛[1]。本研究旨在探讨左旋布比卡因伍用芬太尼在良性前列腺增生摘除术后患者自控硬膜外镇痛效果及循环应激反应的影响。
1 资料与方法
1.1 一般资料:选择ASAI-Ⅱ级,年龄55~75岁、择期作良性前列腺增生耻骨上经膀胱前列腺摘除术80例,随机分为患者自控硬膜外镇痛组(PCEA组)和哌替啶肌注镇痛组(PMA组)各40例。所有患者术前心肺功能正常,无内分泌及严重肝、肾疾患,无硬膜外穿刺禁忌症。
1.2 麻醉方法:术前30min肌注苯巴比妥钠0.1g、阿托品0.5mg。全部病人术中均用连续硬膜外麻醉。选择L2~3行硬膜外穿刺置管。0.33%的卡因维持术中麻醉,酌情静注杜非合剂1.5~2ml,术中维持生命体征平稳。手术结束后将患者送回病房,接监护仪监测生命体征。
1.3 术后镇痛:PCEA组于术毕给予0.25%左旋布比卡因4ml,接PCAD泵作PCEA。镇痛药液为芬太尼0.5mg、氟哌利多5mg和左旋布比卡因187.5mg用生理盐水配至100ml。常规液速2ml/h,追加量为0.5ml/次,锁定时间15min,镇痛时间为24~48h。PMA组:当患者疼痛难忍时,每次肌注哌替啶0.8mg/kg。
1.4 观察指标:①镇痛效果:采用视觉模拟评分(VAS)评定镇痛效果。0分为无痛,<3分为镇痛良好,3~5分为基本满意,>5分为镇痛不满意,10分为剧痛。术后作6、12、24h的疼痛评分。②循环及儿茶酚胺(CA):监测并记录麻醉前、术毕、术后6、12、24h的BP、HR值,并计算心率收缩压之积(RPP),同时采肘静脉血,用高效相色谱法测定血浆去甲肾上腺素(NE)和肾上腺素(E)的浓度。③术后膀胱冲洗量、出血量、膀胱痉挛两组患者例数。④镇痛期间的不良反应。
2 结果
两组患者的年龄、身高、体重、ASA分级、麻醉用药、术中及术后输液量均无显著性差异(P>0.05)。
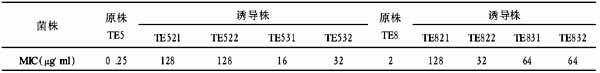
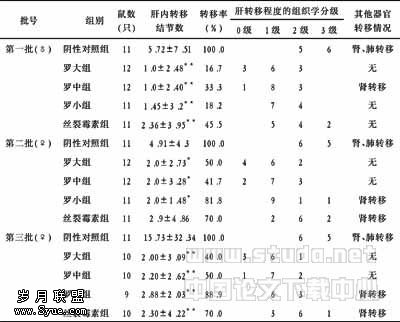
PMA组术后6及12h的VAS评分和术毕相比明显增高,尤以术后6h评分最高,术后各时点的VAS评分PCEA组较PMA组显著低(P<0.05或P<0.01),见表1。
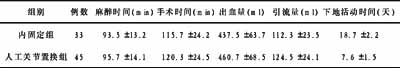
两组患者术毕时HR、RPP、SBP值及CA浓度较麻醉前均明显增高(P>0.05或P>0.01),且PMA组术后各时点的HR、SBP、RPP、CA及术后6、12h的DBP均较麻醉前明显增高(P<0.05或P<0.01),而PCEA组除NE于术后6h较麻醉前高外(P<0.01),其余指标与其麻醉前相比无显著差异(P>0.05)且术后各时点的RPP、血浆CA及术后6、12h的SBP、DBP、HR值均明显低于PMA组(P<0.05或P<0.01),见表2。
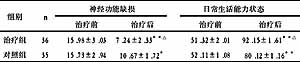
术后膀胱冲洗量、出血量、膀胱痉挛例数PMA组均高于PCEA组(P<0.05),见表3。
两组患者镇痛期间,PMA组有4例出现恶心呕吐,PCEA组有5例轻度嗜睡。
表1 术后VAS评分(略)
与术毕比**P<0.01;与PMA组比△P<0.05 △△P<0.01
表2 血浆CA和循环的变化(略)
与麻醉前比,*P<0.05 **P<0.01;与PMA组比,△P<0.05 △△P<0.01
表3 术后膀胱冲洗量、出血量、膀胱痉挛例数(略)
组间比较:*P<0.05
3 讨论
国人良性前列腺增生症的发病率随着人均寿命的延长,呈逐年上升与欧美国家的发病情况已很相近[2]。其手术摘除为主要方法,甚至被认为是唯一有效的方法[3]术后膀胱冲洗、后尿道手术创伤可能诱导阵发性膀胱痉挛。表现为耻骨、会阴部及尿道外口不适,尿意急迫,肛门坠胀,部分患者出现膀胱尿道的阵发性收缩痛,膀胱痉挛性疼痛发作导致膀胱内压增高,膀胱壁静脉回流障碍,膀胱颈及前列腺窝创缘反复被牵拉,不但增加患者痛苦,也可能引起继发性出血,延长术后膀胱冲洗及留置导尿时间,不利于术后恢复[4]。
左旋布比卡因的优点是体内分布广,清除慢故作用时间长,游离血药浓度低,故中枢神经系统和心脏毒性较小,且心律失常的阈值高,临床安全范围较大[5]。本研究提示:左旋布比卡因伍用芬太尼行PCEA解除了前列腺摘除术后病人的疼痛不适、减弱了术后应激反应、减少膀胱痉挛和术后膀胱冲洗量、出血量,值得临床应用。
:
[1] Sandler AN,strig D,Panos L.A randomized double-blind comparison of lumbar epidural and intravenous fentanyl infusion for postthoracotomy pain relief,analgesic,pharmacokinetic,and respirationeffects[J].Anesthesiology,1992,77:626-634.
[2] 武洪林,李铁强,刘红耀,李保印,主编.老年泌尿外[M]. 北京:科学技术出版社,2001.66.
[3] 顾方六,主编.前列腺病学[M].北京:人民军医出版社,2002.192.
[4] 梅骅,章咏裳,主编. 泌尿外科手术学[M].第2版. 北京:人民卫生出版社,1996.470-516.
[5] 杭燕南,庄心良,蒋豪,等主编.当代麻醉学[M].上海:上海科学技术出版社,2002.385.